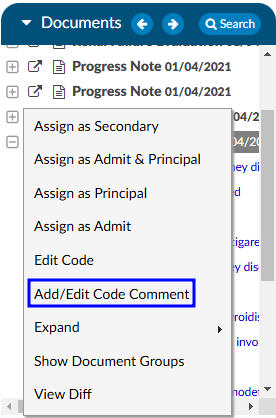
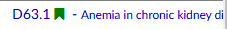
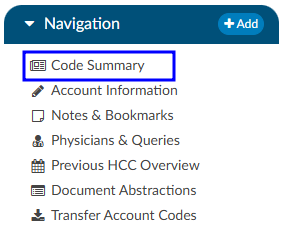
Subsections of Navigation Tree
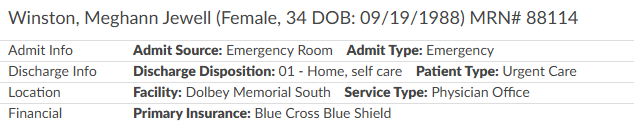
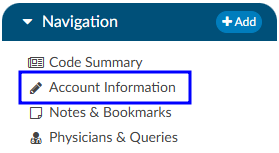
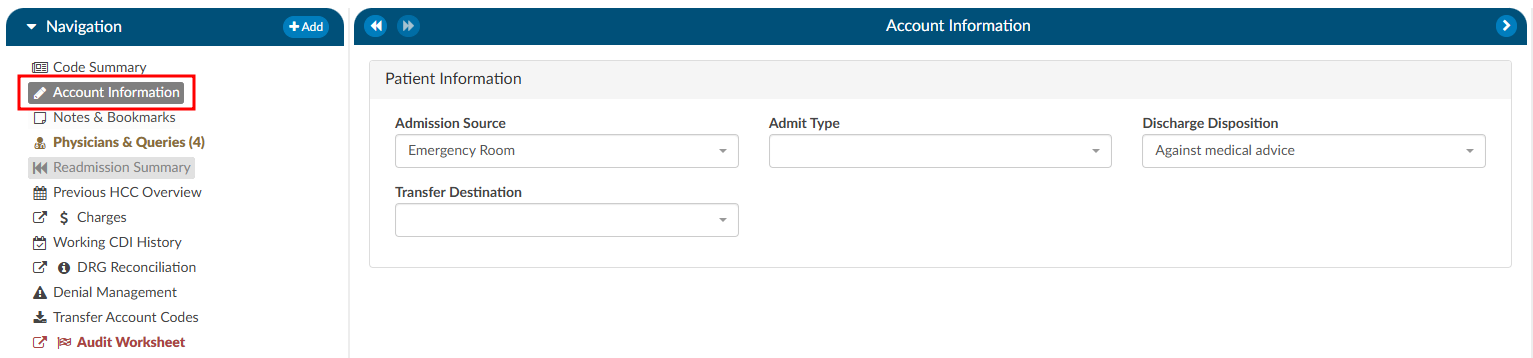
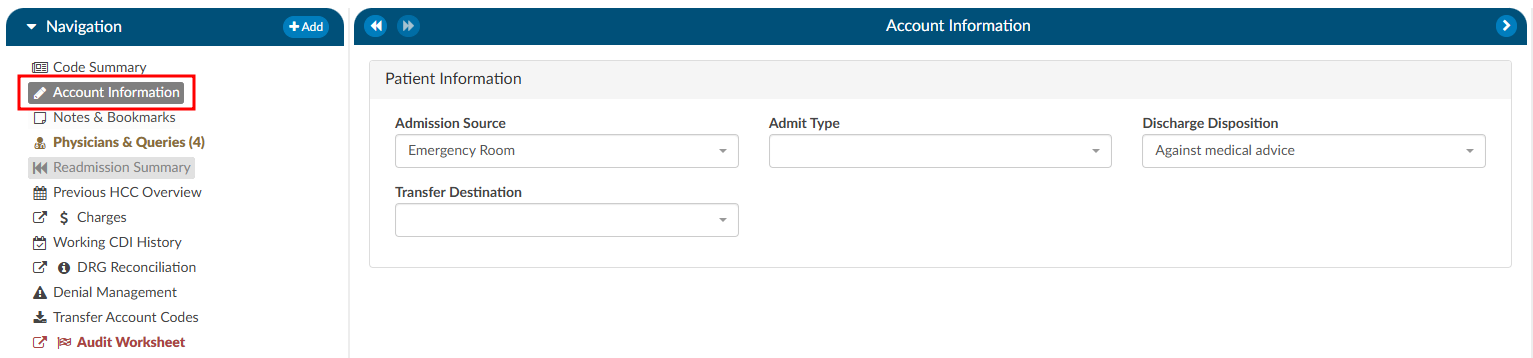
The Account Information tree summarizes patient demographic information (based on custom system configuration) with data captured for purposes of state and/or registry reporting. To update data fields in the Account Information tree, click on the blue button and select the appropriate selection from the drop-down menu.
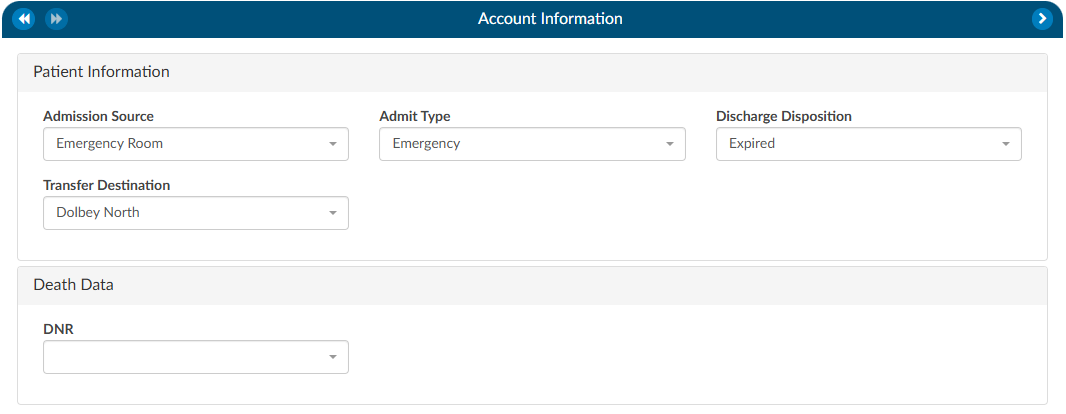
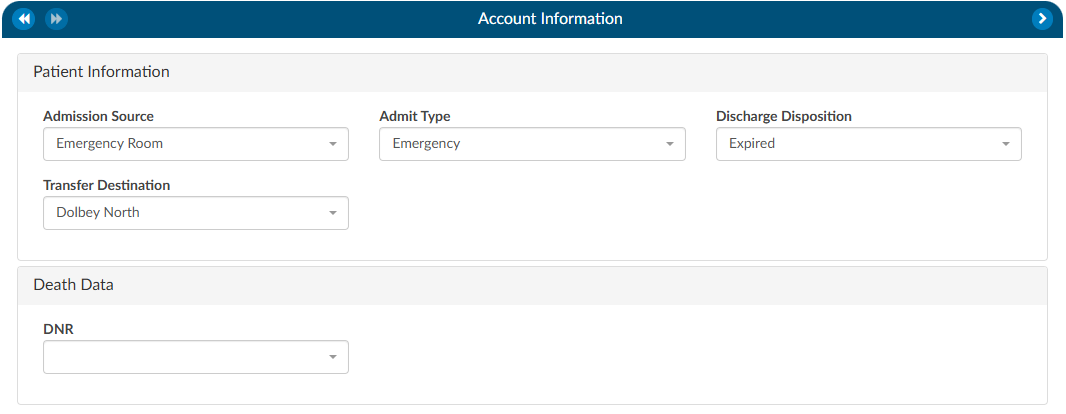
Users can expand the width of the Code Summary tree by clicking on the arrow in the top right corner of the viewer.
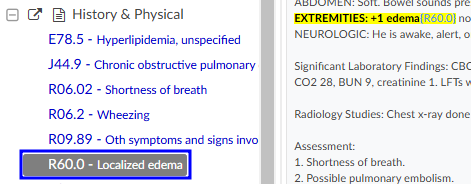
Unspecified Code Edit Flag
On April 1, 2022 CMS made the Unspecified Code Edit effective. This new edit is triggered when a code from the unspecified code list is assigned by a coder. It is the provider’s responsibility to determine if a more specific code from that subcategory is available in the medical record documentation by a clinical provider.
If additional information to identify the laterality from the available medical record documentation by any other clinical provider is unable to be obtained, or there is documentation in the record indicating that the physician is clinically unable to determine the laterality because of the nature of the disease/condition, then the provider must enter that information into the remarks section.
Specifically, the provider may enter “UNABLE TO DET LAT 1” to identify that they are unable to obtain additional information to specify laterality or they may enter “UNABLE TO DET LAT 2” to identify that the physician is clinically unable to determine laterality. If not entered, the claim will be returned.
Fusion CAC/CDI can support the addition of this field to your account information viewer and send the necessary information, known as the billing note, downstream if required. If this is something that you need, please reach out to the Dolbey SME Team at smeteam@dolbey.com.
Add-On Modules and Viewers
Optional Viewers
The following viewers are part of optional
add-on modules
and may not be used at all organizations. If you are unsure if a module is relevant to your
organization, please contact your supervisor. Organizations looking for more information on
these modules should reach out to the Dolbey SME team via email (smeteam@dolbey.com).
Audit Modules
Coding Audit Module (Viewer)
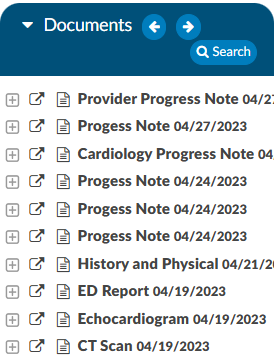
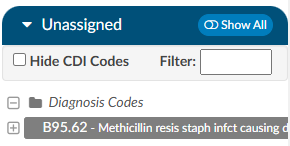
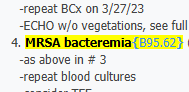
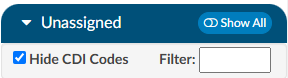
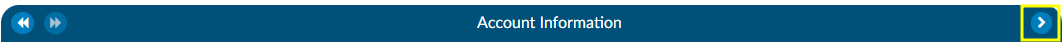
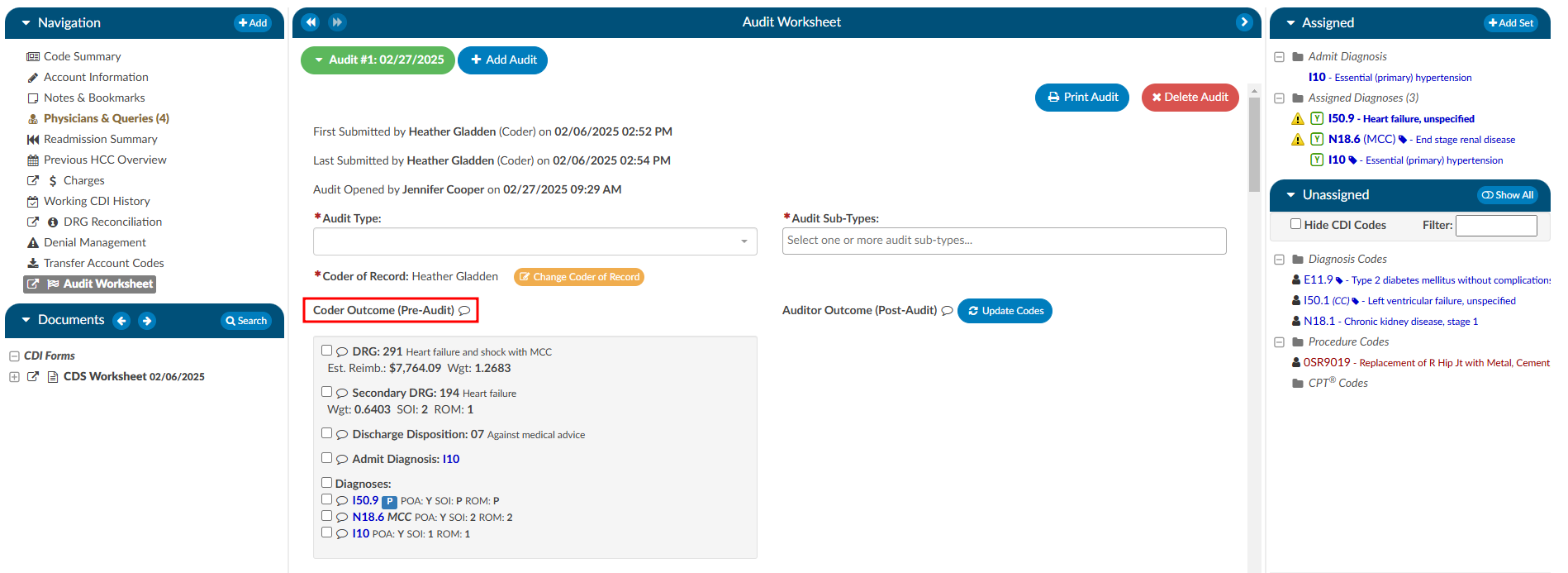
The coding Audit Worksheet displays when the account is opened by a user in the role of Auditor. The Audit Worksheet can be popped out onto a separate screen, allowing the Auditor to have a screen for reviewing the chart. By selecting “Show All” codes in the Unassigned code tree, the Auditor is taken to the documents/documentation supporting that code. This will help streamline the audit process.
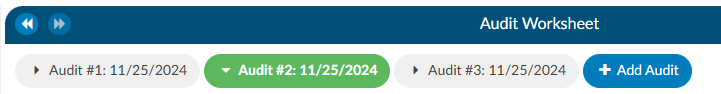
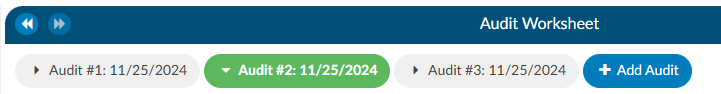
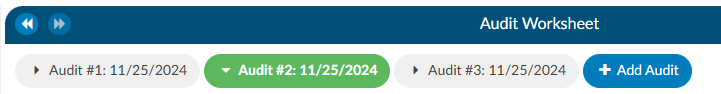
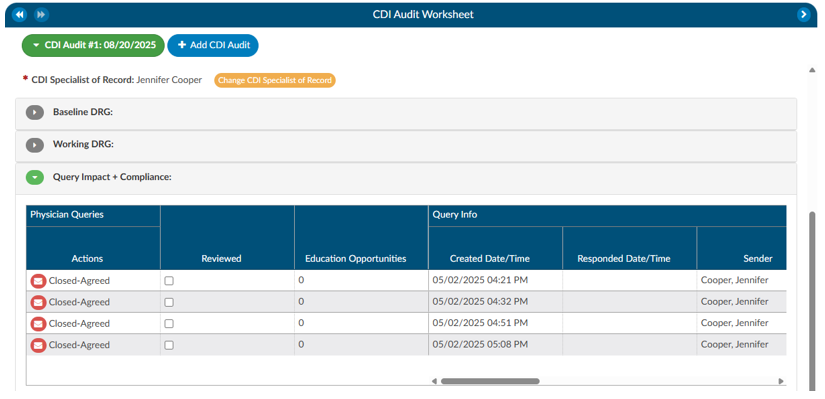
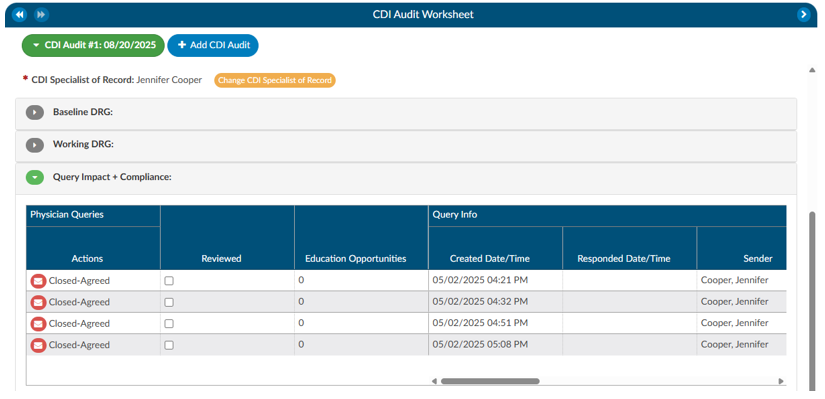
An account can have one or more audits added to it. By clicking +Add Audit a new, blank audit worksheet will be created. These worksheets are numbered and displayed at the top of the audit viewer, along with a date stamp indicating when each worksheet was opened. The worksheet currently being viewed will be highlighted with a green background.
Data in the Audit Viewer is only intended for coder education and administrative staff to score how the Coder is doing in a report card. The Auditor will need to add the Coder of Record so that the Coder of Record, any Auditor, or other user role that has been given access can view the audit worksheets.
The audit module allows for the role of an Auditor within the application. The role of an “Auditor” has the same privileges as a “Coder” when it comes to account editing. More details on audit functionality can be found in the Audit Worksheet section.
Aduit Worksheet Permissions
If needed, the Audit Worksheet can be seen by a CDI Specialist. The CDI Specialist would only have the option to view and print. All editing, routing, and deleting abilities are not available.
Please contact the CAC Support Team to opt-in to this permission at cacsupport@dolbey.com
CDI Audit Module (Viewer)
The CDI Audit Module is a tool designed to help CDI auditors evaluate the quality, accuracy, and compliance of CDI work within a patient chart. It provides a structured workflow to review whether the baseline DRG was assigned correctly, whether the final working DRG reflects appropriate documentation and coding practices, and whether queries sent by CDI professionals followed compliance standards.
Audits can be conducted at different stages of the patient’s stay. A concurrent audit allows you to evaluate a case while the patient is still admitted. A post-discharge audit can be performed once the case is complete, ensuring that no documentation opportunities were missed. Finally, the module also supports retrospective random audits, which can be used to evaluate CDI quality as part of regular compliance monitoring. This flexibility ensures that audits can be integrated into both day-to-day CDI operations and broader quality assurance programs.
Prerequisites
Before starting a CDI audit, two requirements must be met:
- CDI Auditor Role: You must be assigned the role of CDI Auditor within the system. Without this role, you will not see the CDI Audit worksheet or be able to launch an audit.
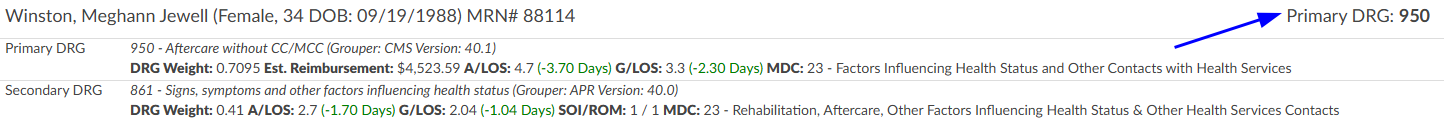
- Patient Chart with a Baseline DRG: The patient chart must have at least a baseline DRG already assigned by a CDI user. This ensures there is an initial point of comparison for your audit.
If either of these prerequisites is missing, the system will not allow you to proceed with the audit.
More details on audit functionality can be found in the CDI Audit Worksheet section.
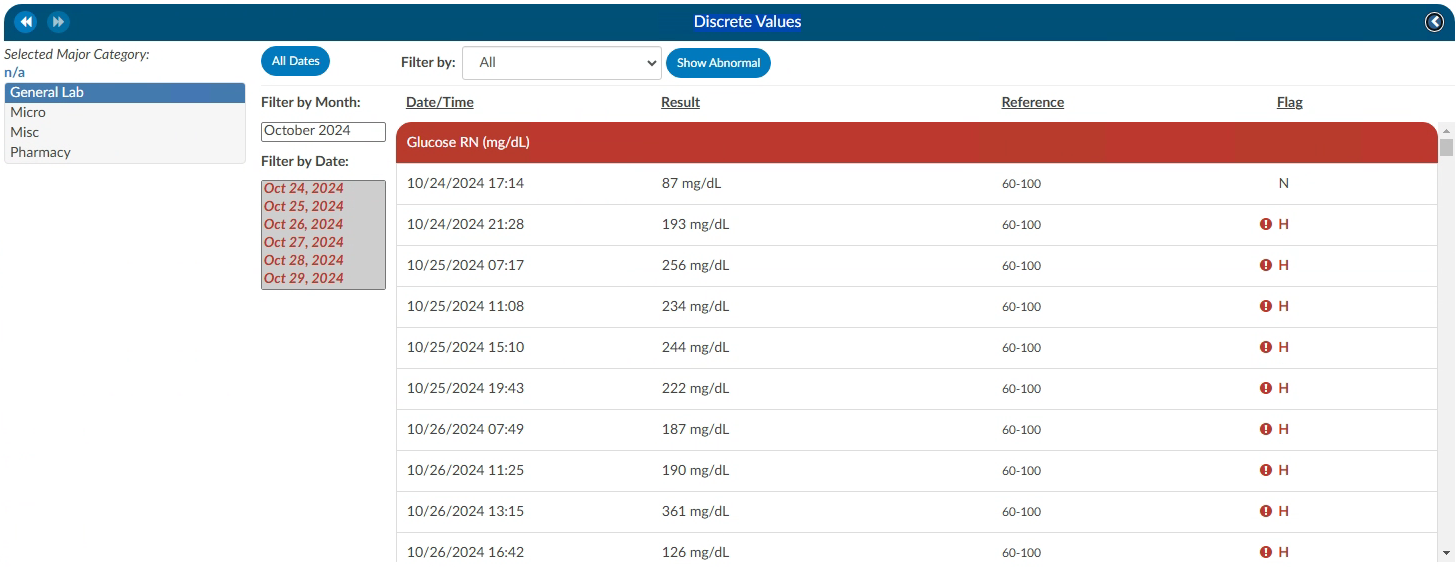
Discrete Values (Viewer)
This feature may not be supported by your organization’s EHR vendor. The Discrete Values viewer show trending data or data that has values. The most common examples of discrete values are lab values and vital signs. The viewer can be popped out into another window by clicking on a little square with an arrow pointing to the right in the navigation tree next to the viewer name.
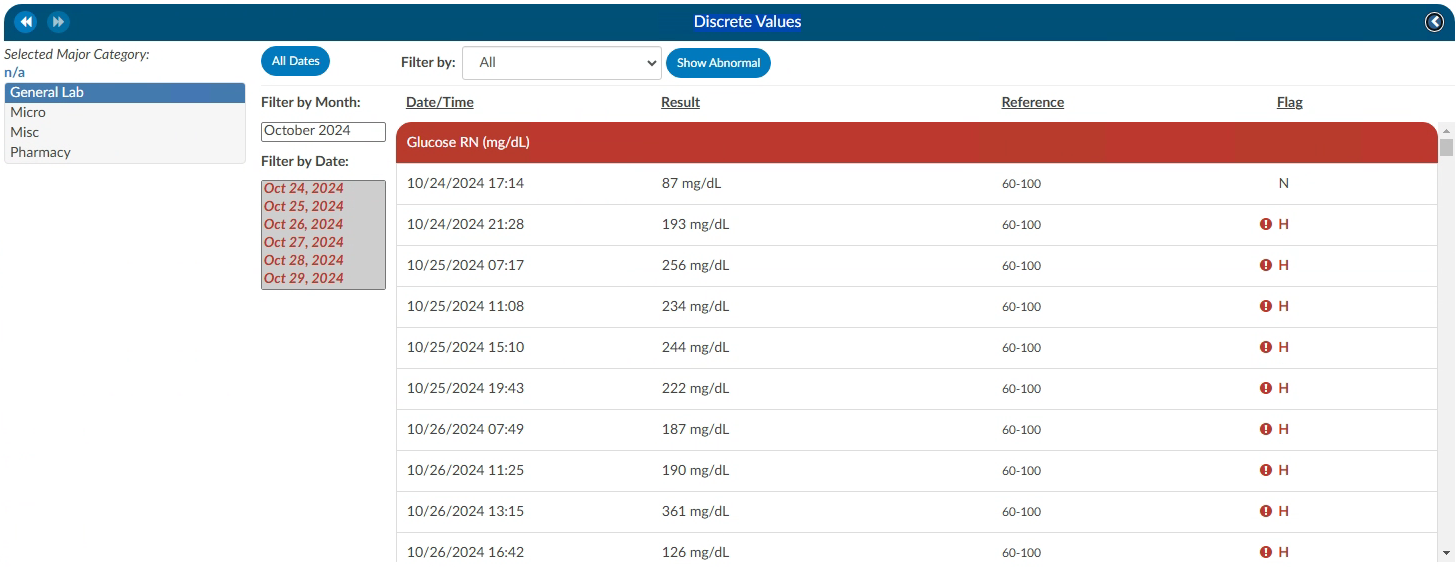
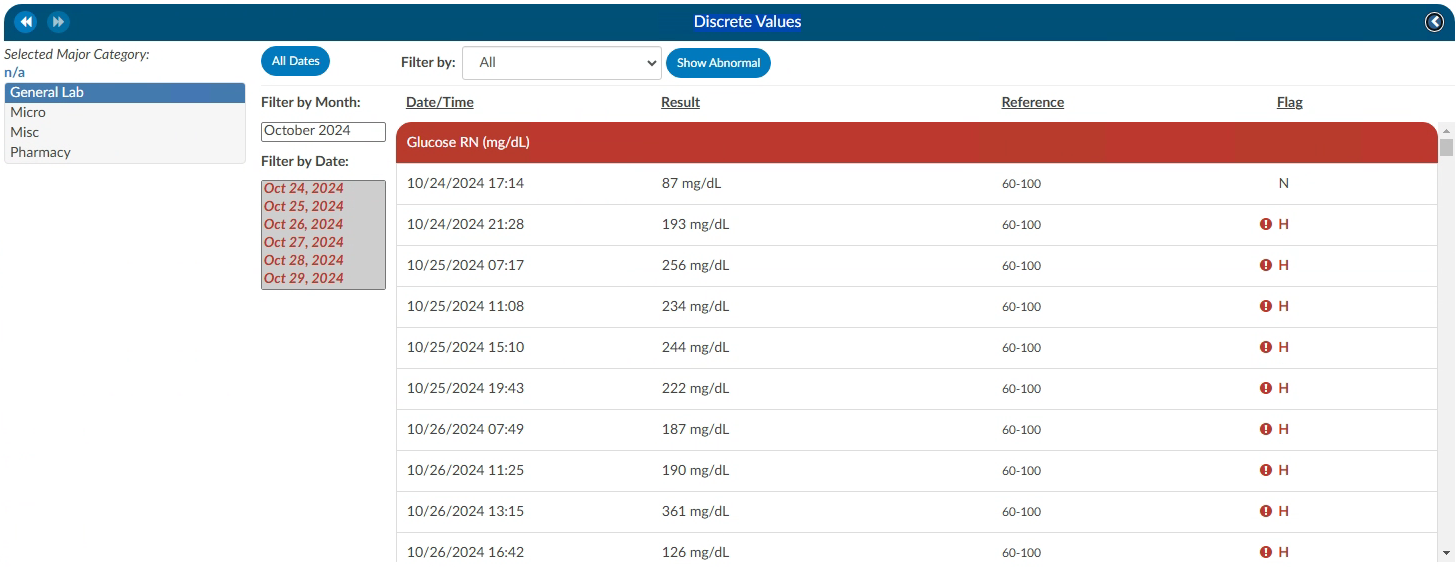
An older style of discrete data can be displayed in a Discrete Values viewer. Tabs across the top of the screen display the categories of data. This displays each of the types of discrete data elements, which may vary by organization.
The Discrete Values viewer has a Filter by Month box, listing the months that contain values. Selecting a month will highlight all the corresponding dates in the Filter by Date box. The resulting values will show in the viewer. The Normal and Abnormal tabs both have this functionality and are filtered separately.
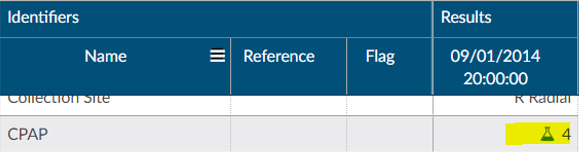
Discrete Values with a grey header are within normal limits. Each organization sends what is the reference point to determine what is normal and what is abnormal. If a header is display in red, it is considered abnormal by the organization. In addition to the header color, users can tell if the value is out of normal limits as there is a flag that indicates if the value is low vs. high.
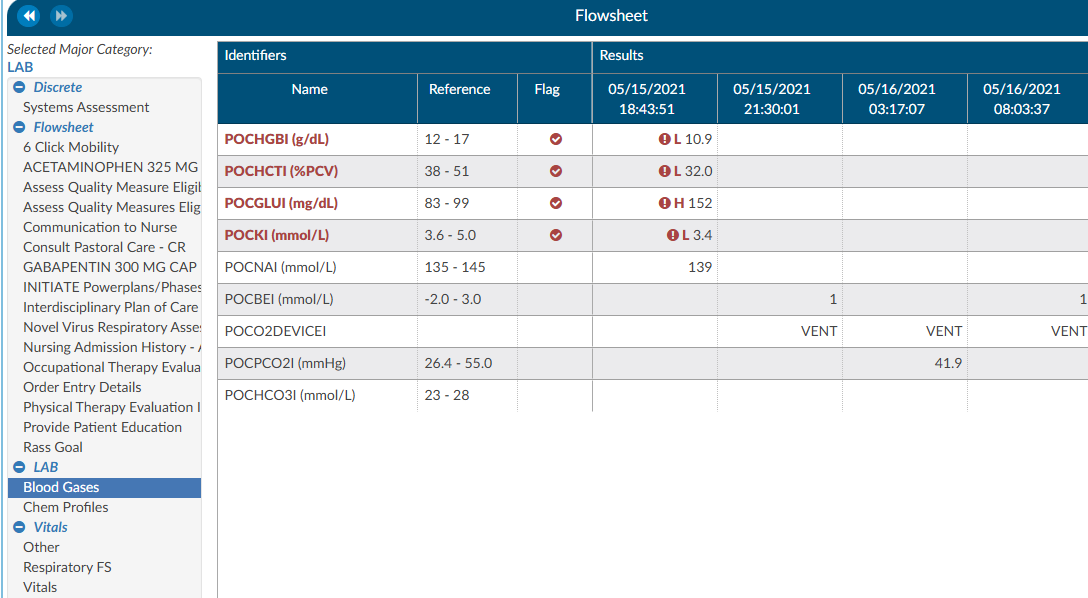
Flowsheet (Viewer)
This feature may not be supported by your organization’s EHR vendor. The Flowsheet viewer shows information found in nursing documentation such as nursing or respiratory assessments, skin assessments, intake and outake data, etc. The viewer can be popped out into another window by clicking on a little square with an arrow pointing to the right in the navigation tree next to the viewer name.
The Flowsheet viewer is the most recent style of discrete data viewer. This viewer is organized much like a spreadsheet. Depending on configuration, users may see major categories on the left-hand side of the spreadsheet (there are many different options as each site is a little different.). Upon clicking on one of these items users will be presented with a grid to the right. That grid will have multiple columns, the first column being name. Hovering over the column name will display three little lines. Clicking on them, will allow the user to filter in order to narrow down the data. If any of those names appear in red that means that at least one of the data elements are outside of the normal limits if there is a range.
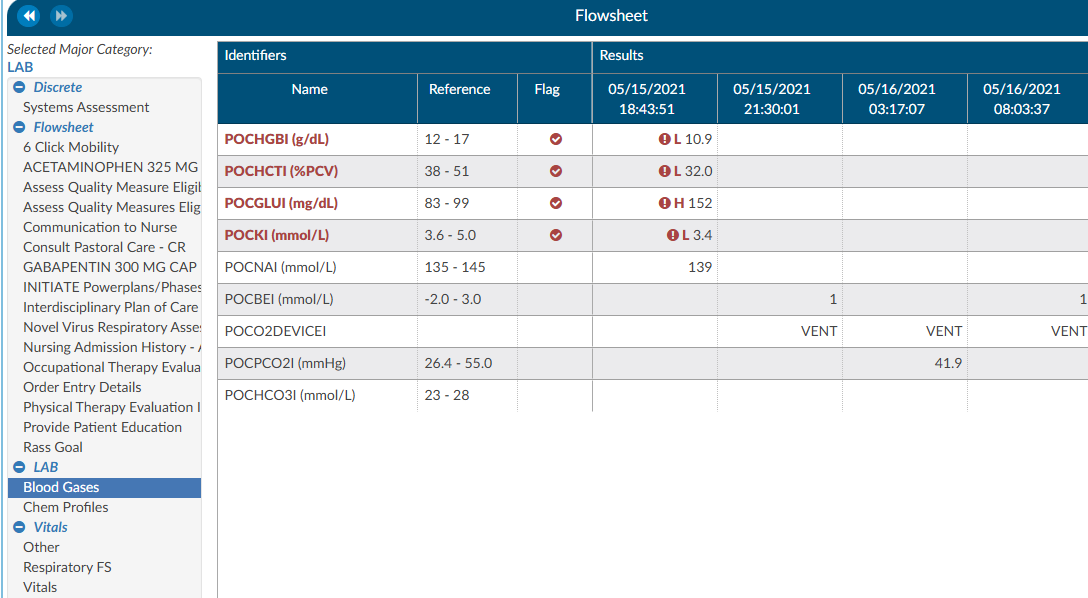
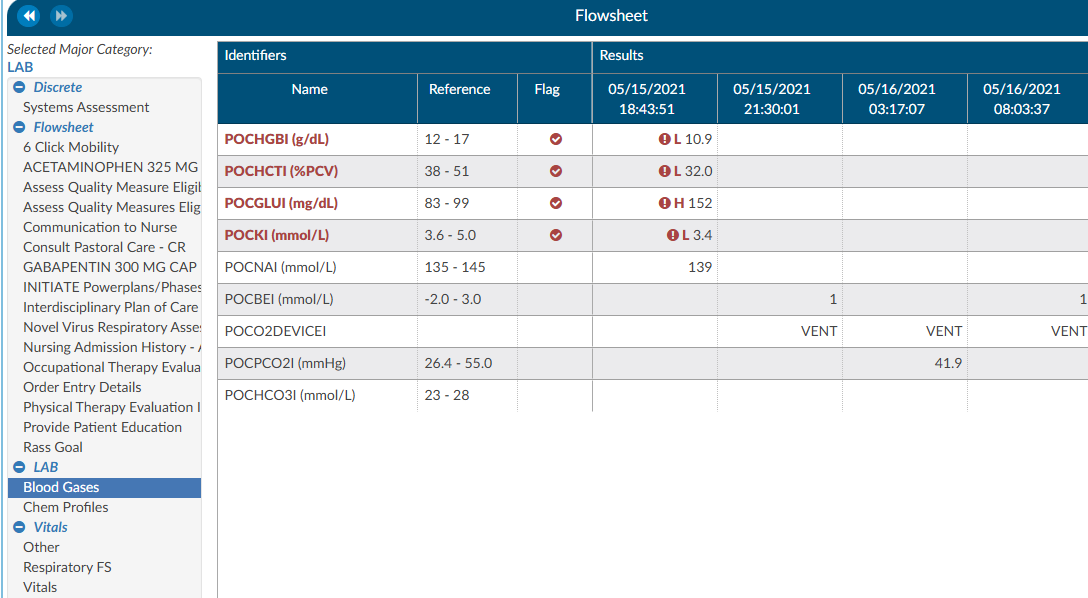
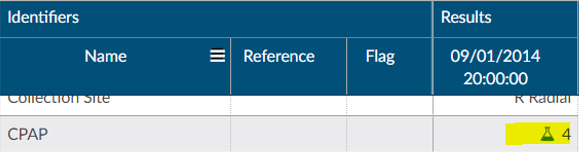
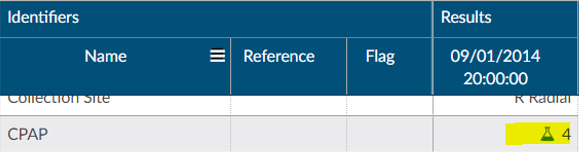
To the right of the name, if applicable, is a reference column. This reference column will indicate if the value is within normal limits. This is data that the EHR system has sent to Fusion CAC. If the reference column is available, then to the right of that is a flag column. A checkmark in that field also means the value is out of the normal range. This column can also be filtered if the user wants to look at everything outside of the normal limits. Next to that field is a date and time column. The user may see multiple dates and times depending on how the data is organized and how frequently it is documented. If a discrete value on the Flowsheet viewer has a specimen, it will show as a beaker symbol in the Results column. Hovering over the symbol will provide the name and site of the specimen.
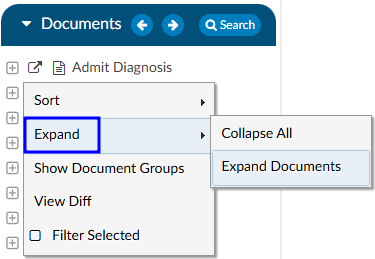
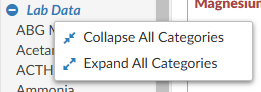
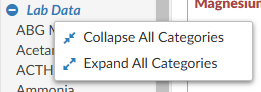
Right clicking in the Major Category column will show a menu allowing the user to expand or collapse all categories. That configuration will be saved for all accounts that have the Flowsheet Viewer, per user role. Note that if a user collapses/uncollapses a major category in the pop-out, it will not be seen on the main page until the user moves to a different viewer and back.
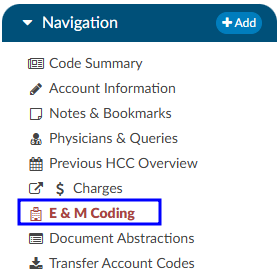
ER E/M Module
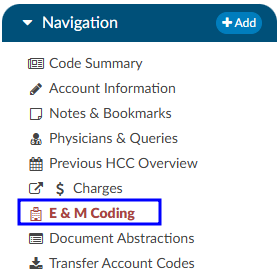
The ER E/M viewer is part of an add-on module for any chart with a “Is Emergency” flag within the account properties.
If this module is turned on, any “Is Emergency” chart will have the “E/M Coding Worksheet” in the Navigation menu.
There are several sections to the E/M Coding worksheet including: E/M No Charge, E/M Level, Trauma, Critical Care, Medications, and Additional Charging. More details on ER E/M functionality can be found in the Administrative User Guide.
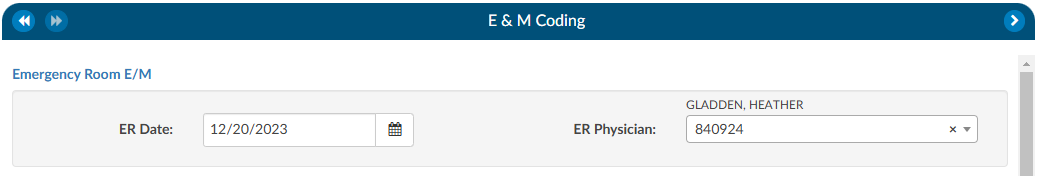
Completing the ER E/M Worksheet
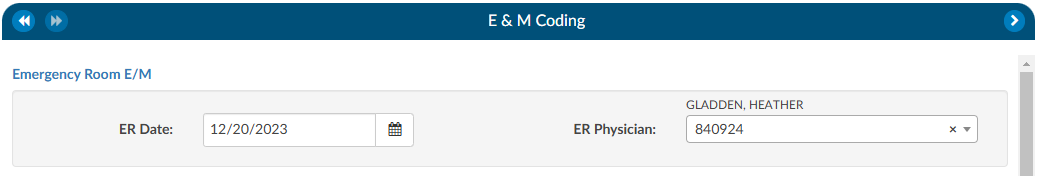
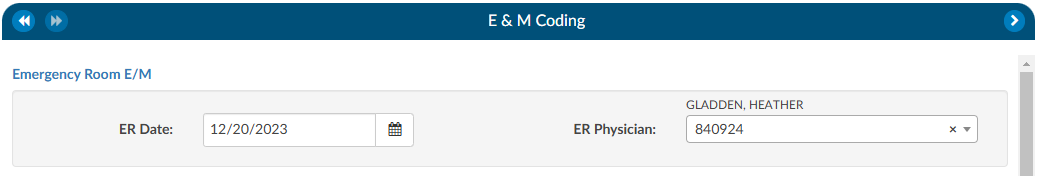
ER Date and Provider
The first step in completing this worksheet is filling in the ER Date and the ER Physician fields. Once these are completed, the rest of the worksheet will populate.
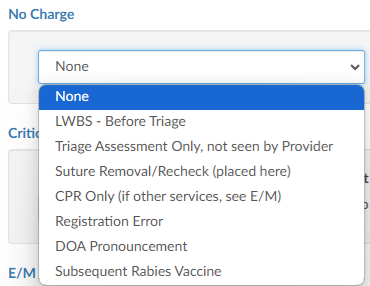
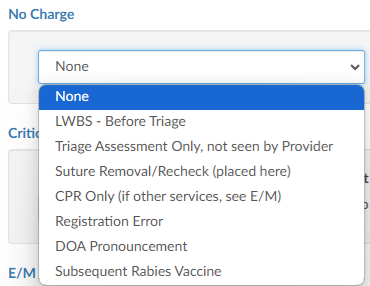
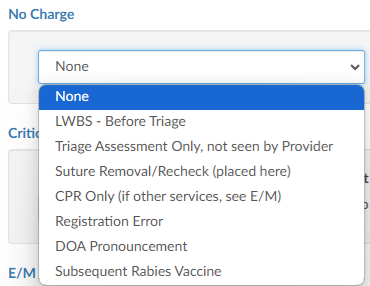
No Charge
If a patient fits the criteria for “no charges” (for example, a registration error), all other fields in the worksheet go away because there is nothing else to be done from an ER charging perspective. However, other selections from the list will populate the fields accordingly.
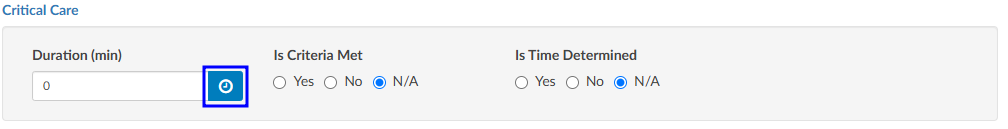
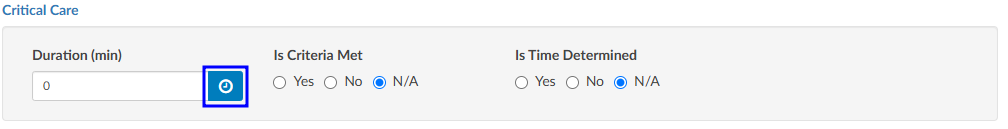
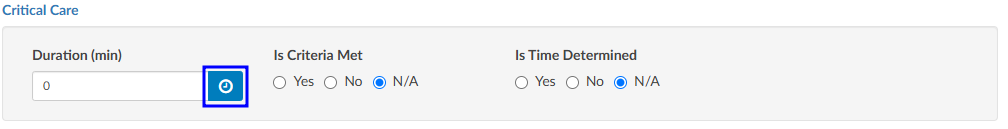
Critical Care
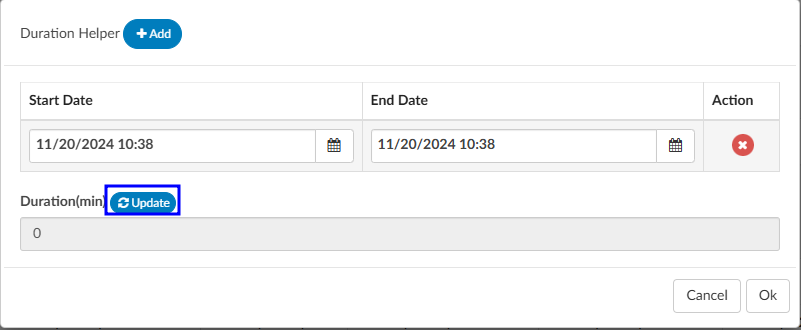
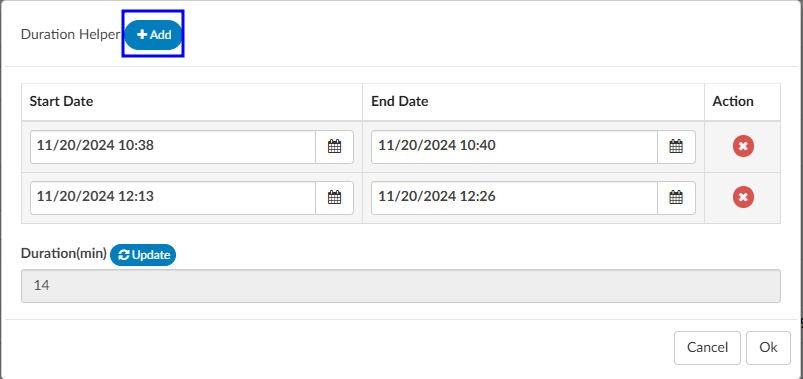
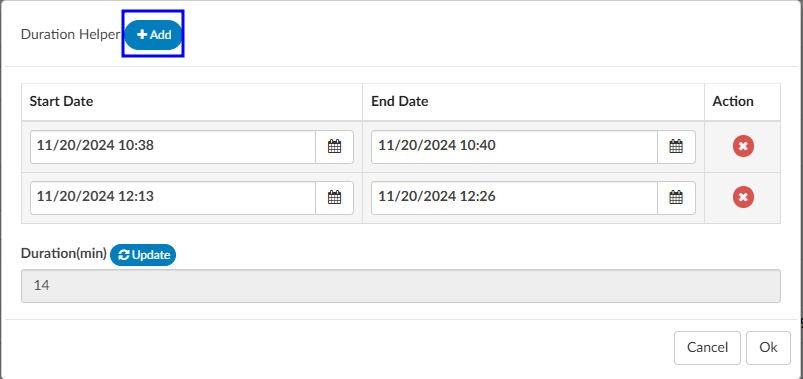
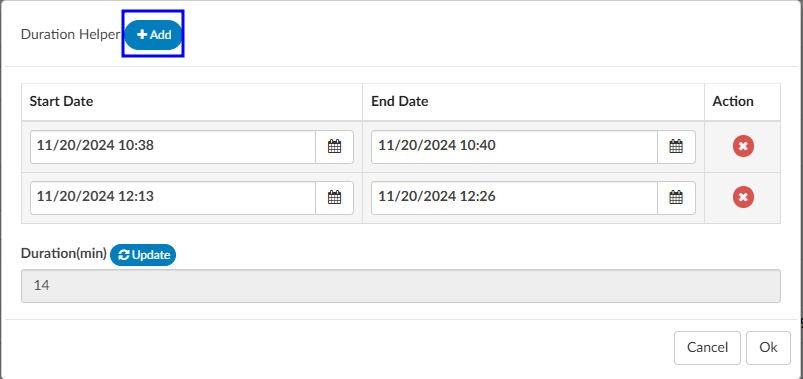
Select appropriate answers to “Is Criteria Met” and “Is Time Determined.” To enter the duration, click on the clock icon.
Enter start date/time and click on the Update button for the minutes to display.
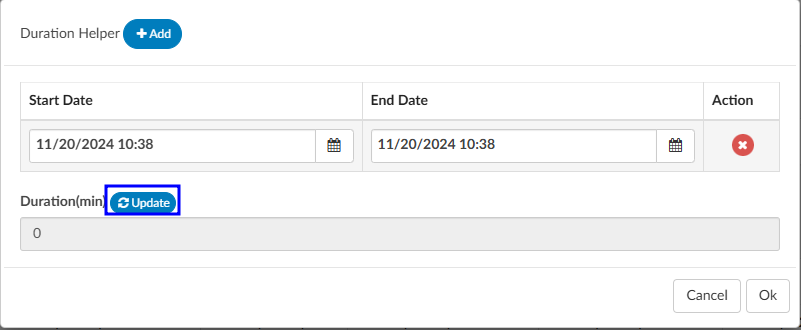
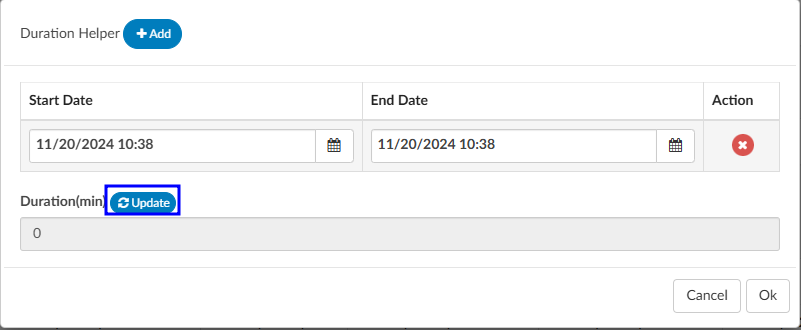
If there were multiple spans of time for critical care, click on +Add and enter any additional durations of time. The system will add up on the minutes and display once “Update” has been selected.
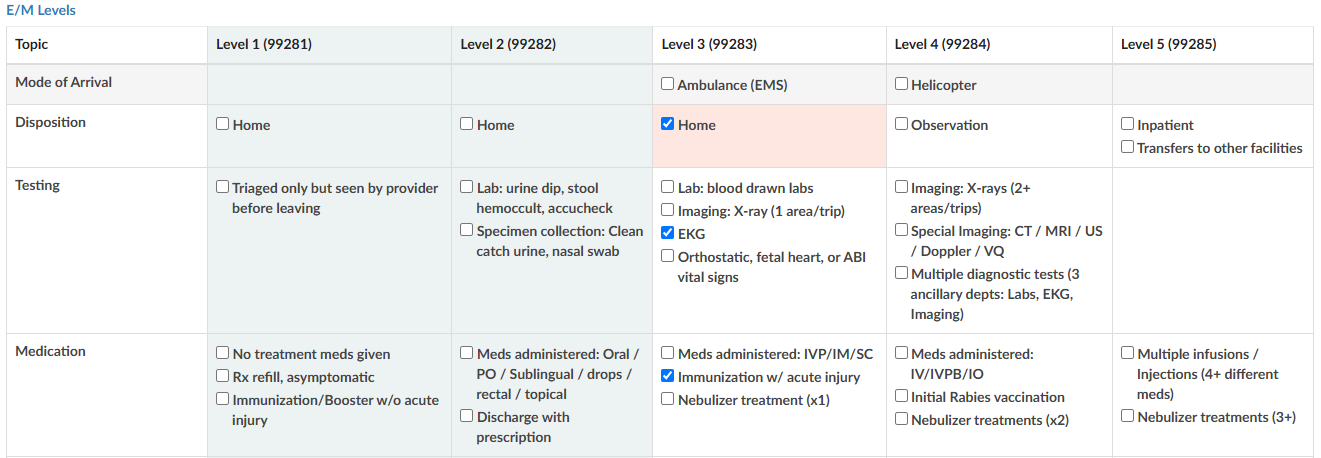
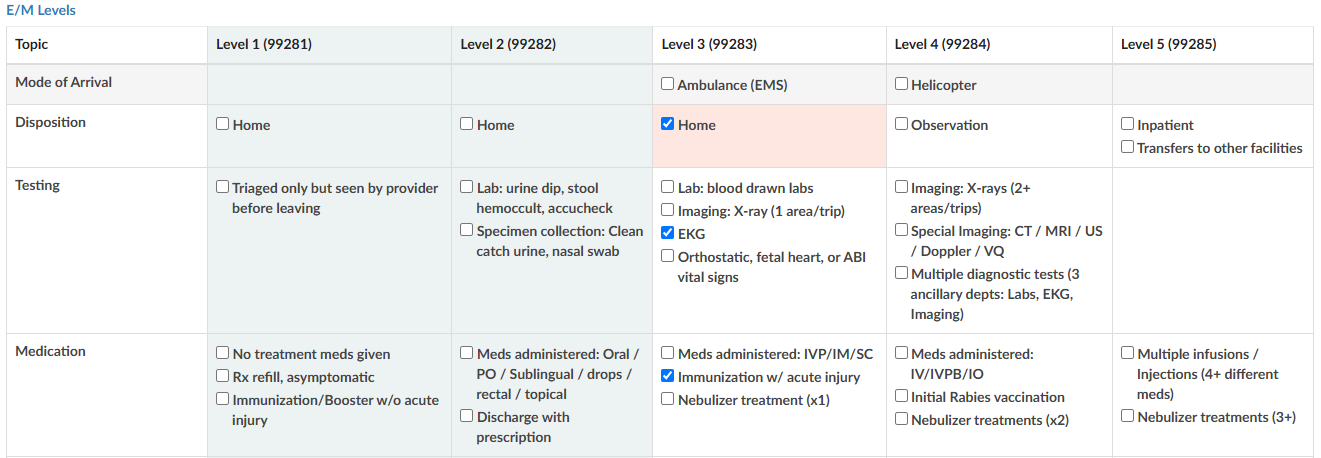
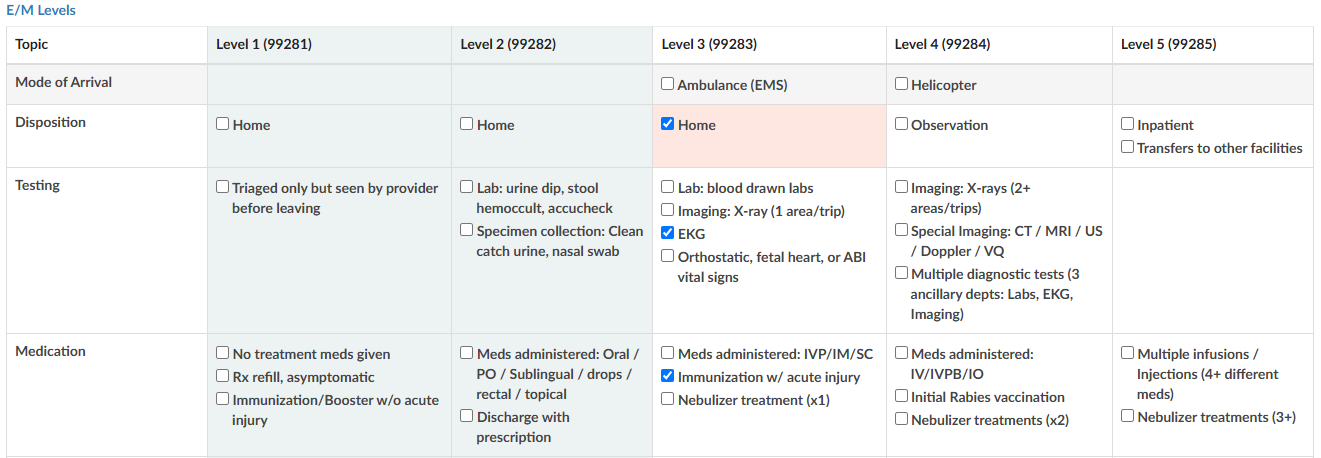
E/M Levels Matrix
The E/M Levels martix is configured per organization. This matirx will allow the user to check what interventions were completed during the ER visit. Once an intervention is selected from one of the columns, that becomes the minimal level and all columns before that will gray out. As the remaining sections are completed, users may see the level advance.
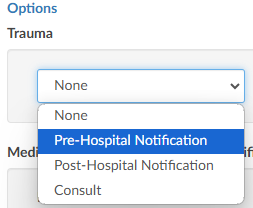
Trauma
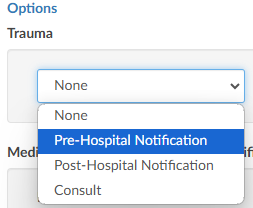
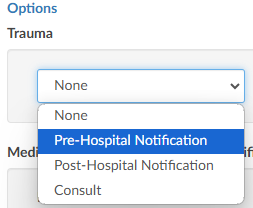
If the case was a trauma, make the appropriate selection from the dropdown menu (pre-hospital notification, post-hospital notification, consult).
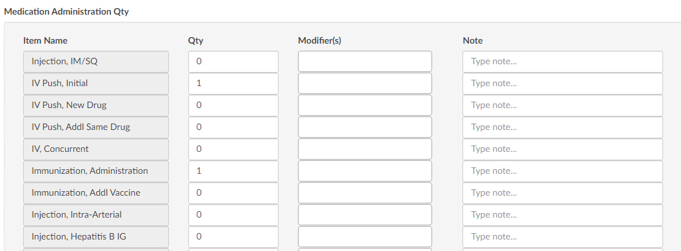
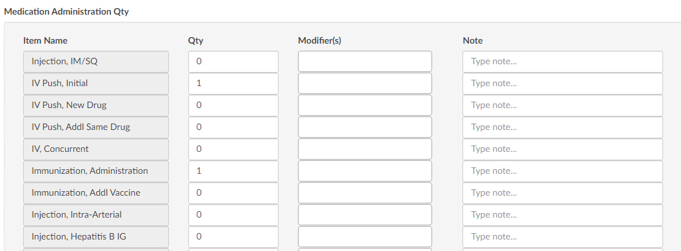
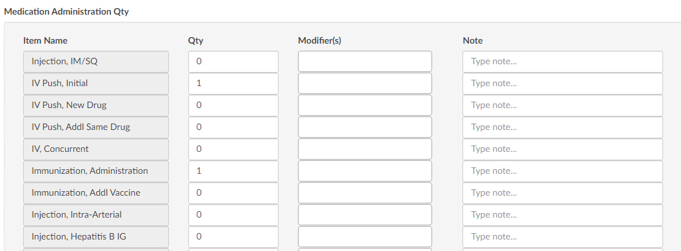
Medication Administration Qty
Based on the selection, additional fields or boxes will populate. Complete the quantities, add modifiers, and any notes. Modifier fields are available in the appropriate sections of the worksheet. The user can add up to four (4) modifiers unless they are using the Solventum CRS encoder, then they will be able to add up to five (5) modifiers. The “Notes” field is available for the coder to track things such as medications.
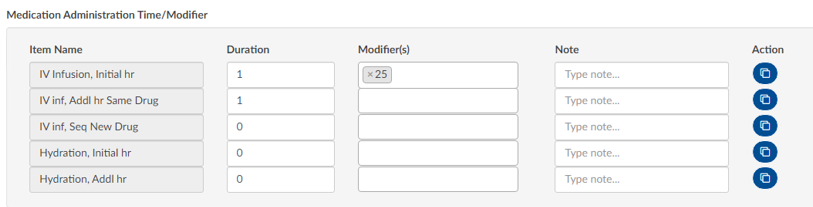
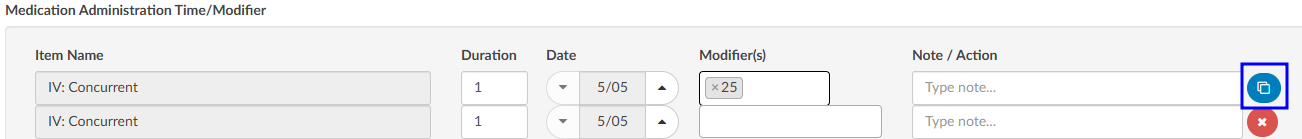
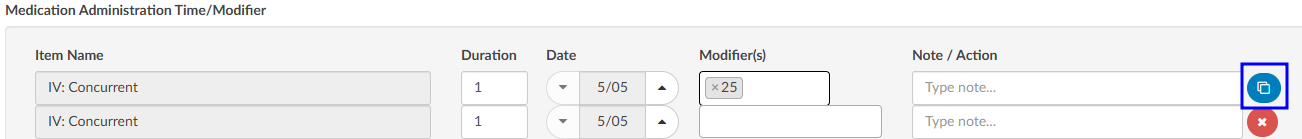
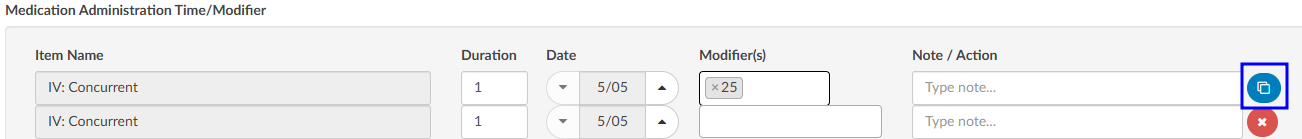
Medication Administration Time/Modifier
Update this section with the duration of each medication as needed, any modifier(s), and notes. The user can add up to four (4) modifiers unless they are using the Solventum CRS encoder, then they will be able to add up to five (5) modifiers.
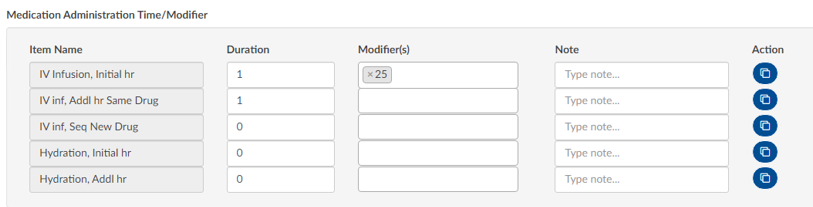
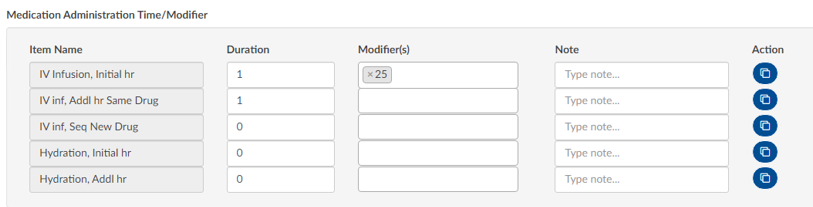
If there are multiple infusions (for example, one infusion started in left arm and one infusion stated in the right arm), click on the Action button to create another row to be completed including appropriate modifiers for each infusion.
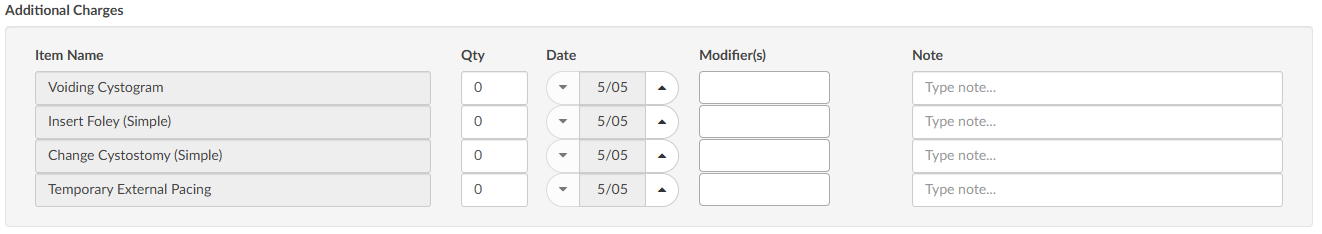
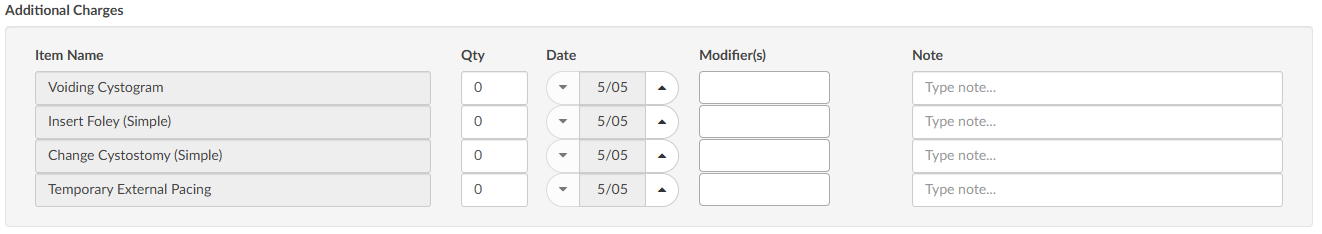
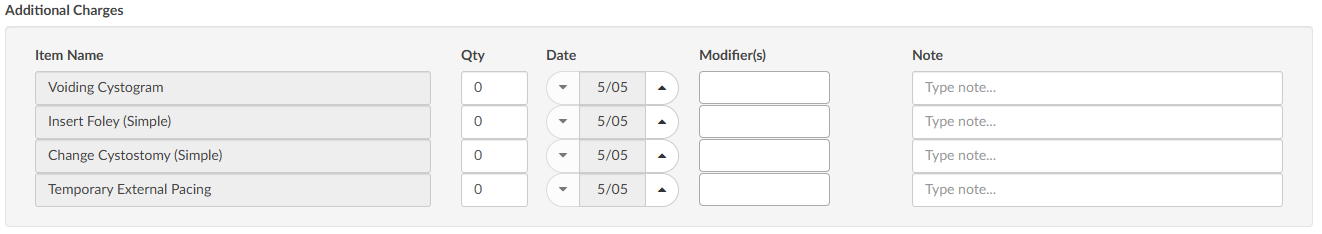
Additional Charges
Add any additional charges. Much like the matrix, the additional charges section will be configured per each organization to include the necessary charges each organization captures.
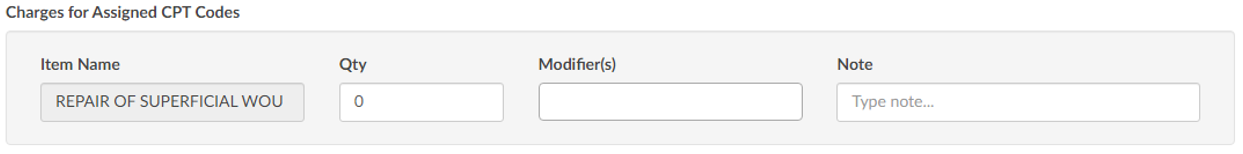
Charges for Assigned CPT Codes
If the Coder adds a CPT code (otherwise referred to as “soft code”), the codes will appear in this section of the E/M Coding worksheet. It must then be determined by the Coder, or Charger, if the procedure added by the Coder occurred in the ER and should be charged. If so, the fields should be completed. If the procedure is determined to have occurred elsewhere, leave the 0 in the field.
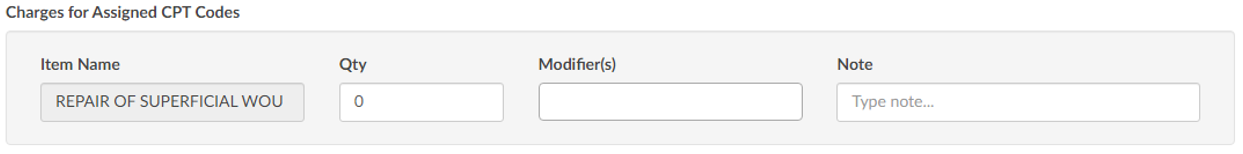
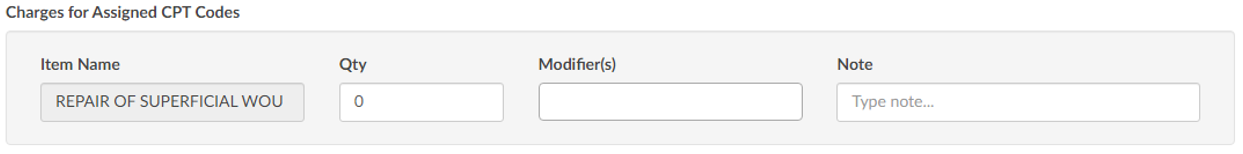
Note
When there is a CPT coded added that has no CDM charge, it won’t appear in this section; only those that have a CDM.
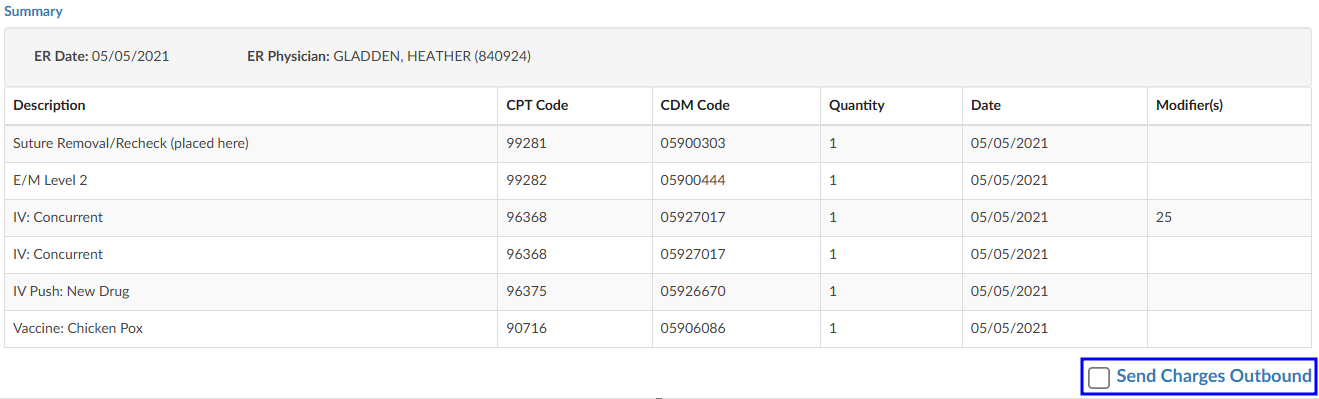
E/M Summary
Once the Additional Charges section is complete, users will see the Summary which details the E/M level and other charges with the corresponding CDM Code.
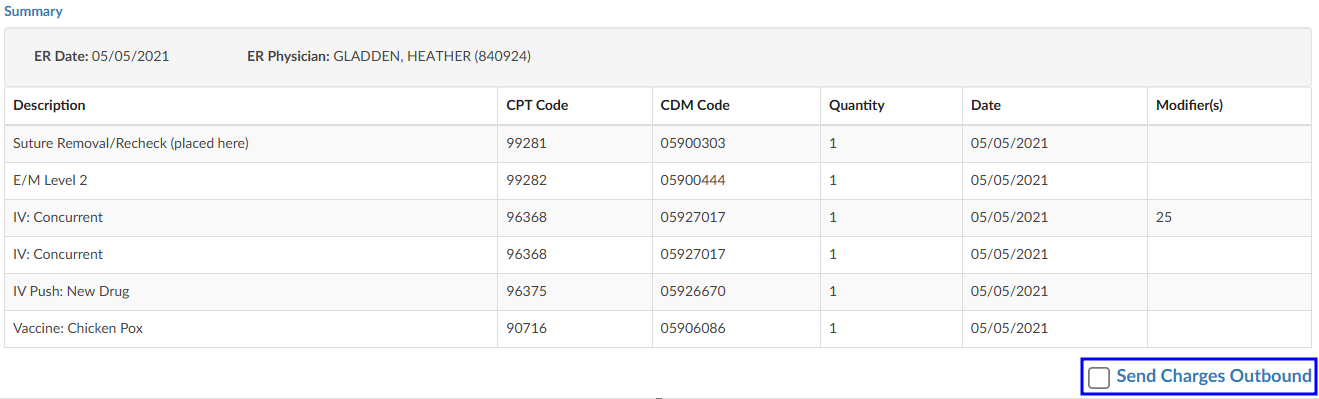
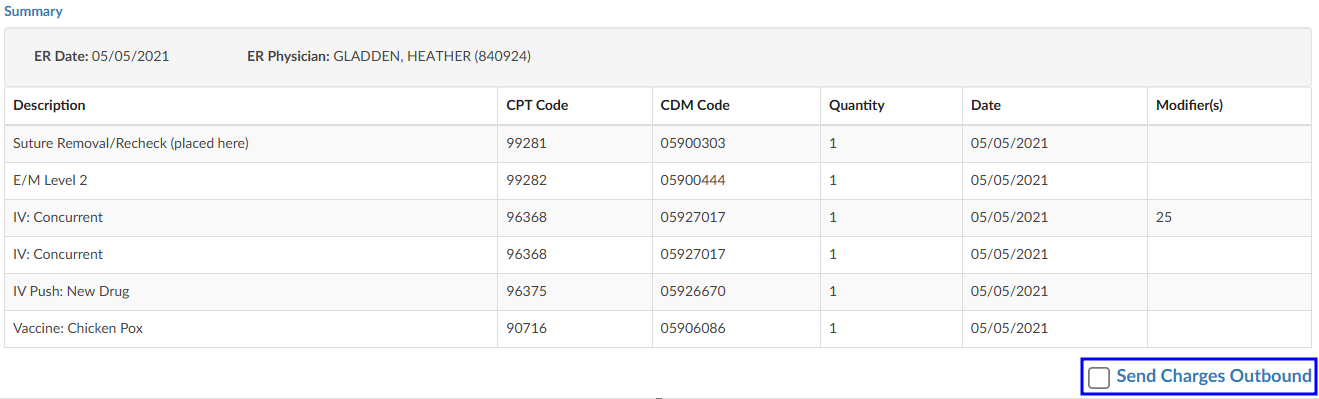
When all charging is complete and the charges are ready to be submitted, check the “Send Charges Outbound” checkbox and click on the Save button in the banner bar. This action sends charges out and the account will automatically route to a coder worklist so the rest of the coding that is not charge-related can be completed.
If the charges cannot be completed for some reason (missing trauma documentation), the box should NOT be checked, and instead, a pending reason should be assigned on the Code Summary. Once a pending reason has been added, click on the Save button in the banner bar.


If the “Send Charges Outbound” checkbox is NOT checked, the Coder will get a warning that ER charges are missing and will not be able to submit the account upon completion of coding. The Coder, in this case, would attach a pending reason to send the account back to the user applying charges to check the box. The account then goes back to the Coder to submit the account for final billing. This workflow ensures that the Coder does not submit an account unless all ER charges have been completed.
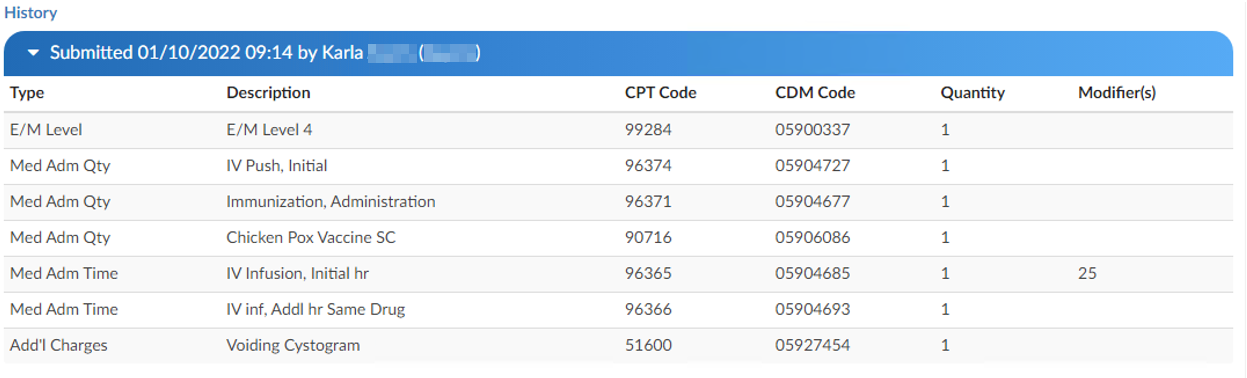
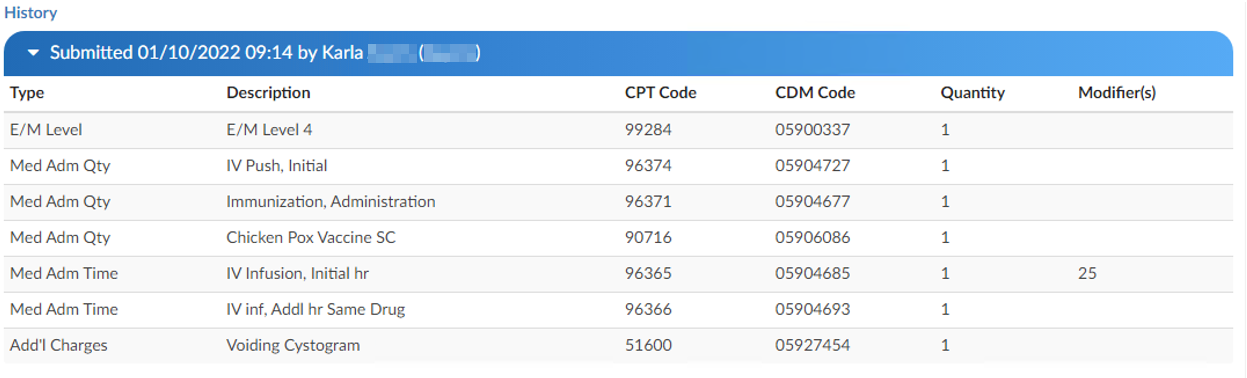
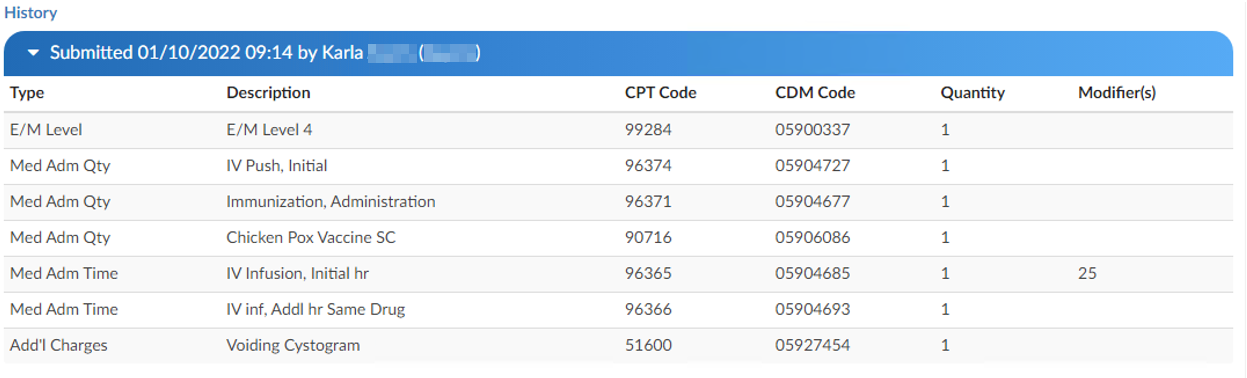
E/M History
This section displays the history of charges submitted.
Click to expand for details.
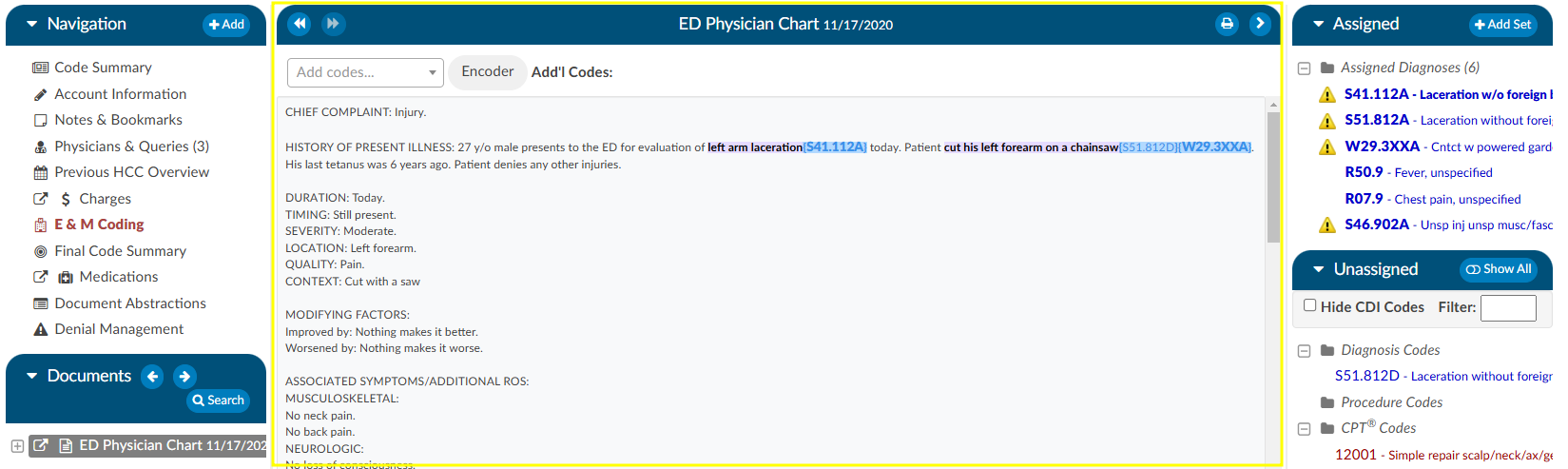
Physician Coding/Single Path
Physician Coders differ from hospital coders in that they will usually work for a doctor who specializes in a specific type of medicine. As a result, they typically code for just that specialty. These coders will only deal with a subset of the ICD10 code set. Within the CAC system, functionality is built to allow a Physician Coder to code charts just like hospital coding staff. The Single Path coding role allows the user to code an account as a final coder and a physician coder simultaneously. When a Single Path user opens up the detail on a CPT code, they will see two separate fields for modifiers, and they can enter modifiers for both.
A Single Path role can also be modified from the Profile drop-down menu under the user name at the top of the Account Detail screen, provided that another changeable profile role, such as CDI, Coder, or Physician Coder, is available on the User Profile. When adding or editing modifiers in the Charges viewer, the Single Path user sees the Coder’s version of the viewer, so what is added will be viewable to both a Coder and a Single Path user. The Physician Coder charges viewers are different and viewable only to them.
Audit Worksheet
Starting an Audit
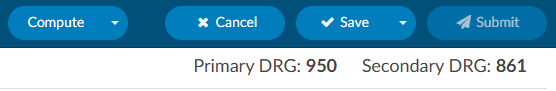
The pre-audit codes and DRG are displayed for easy reference by the Auditor. The Auditor conducts the review (see steps 1-9) and makes changes to the codes in the Assigned code tree.
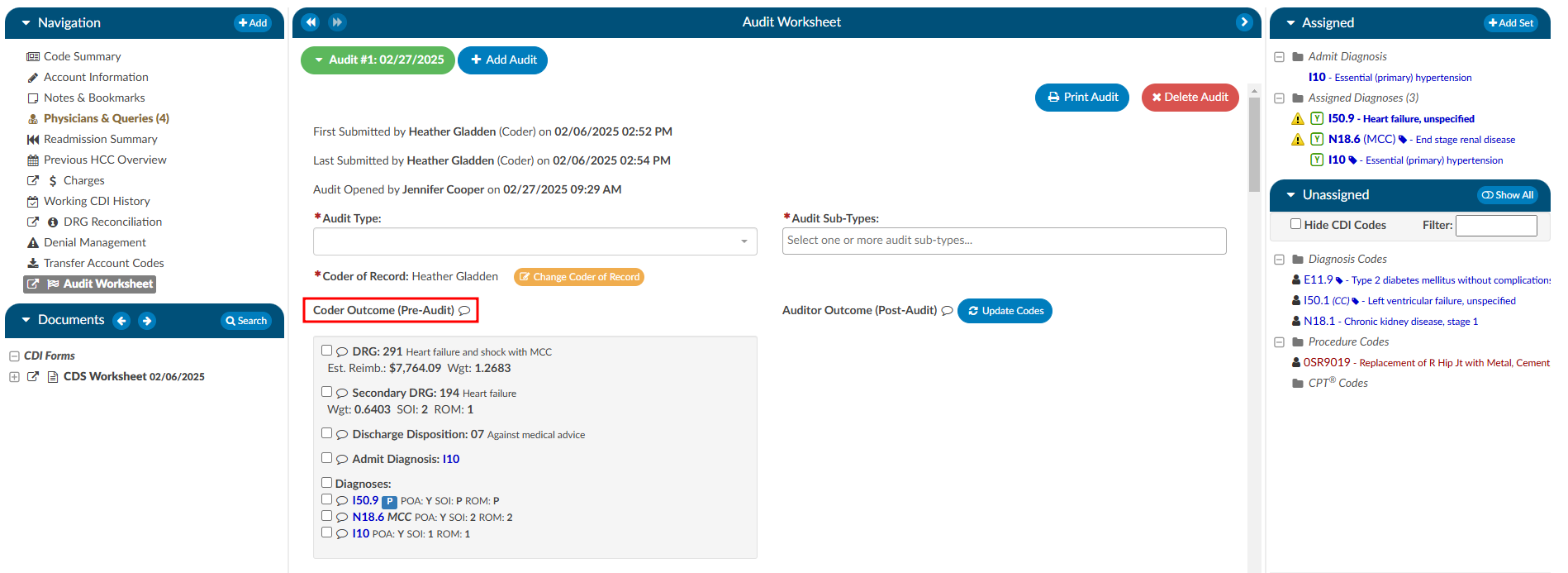
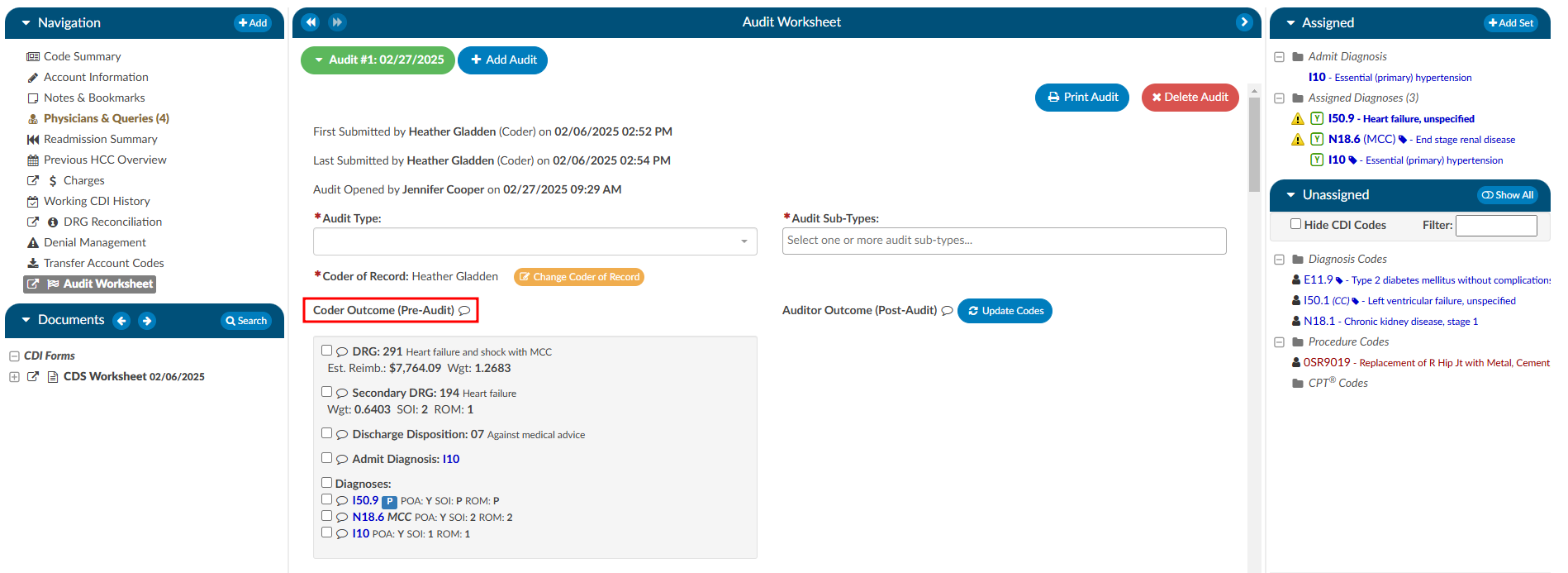
Step 1
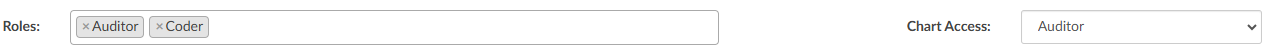
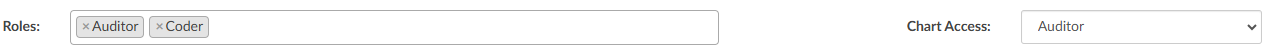
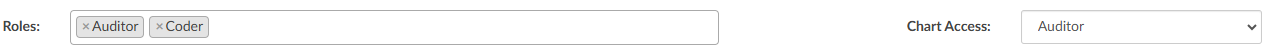
Ensure the current user role is set to have the Auditor role as well as Chart Access of Auditor.
Step 2
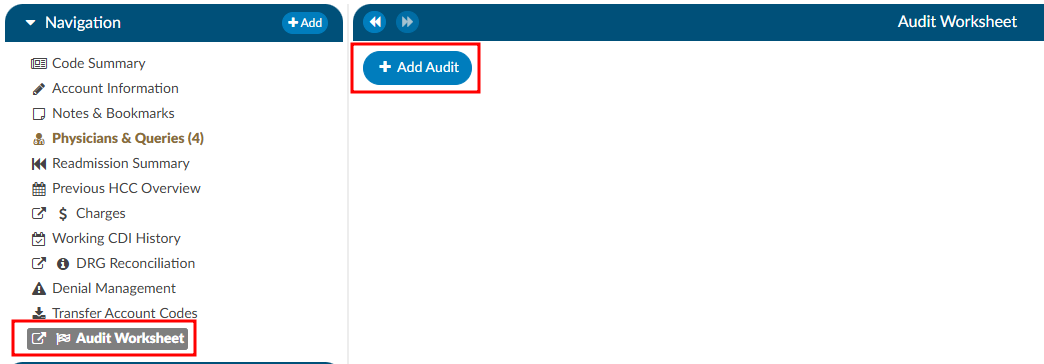
Open a chart that has been submitted by a Coder. This may come from a worklist or by manually typing in an account number.
Step 3
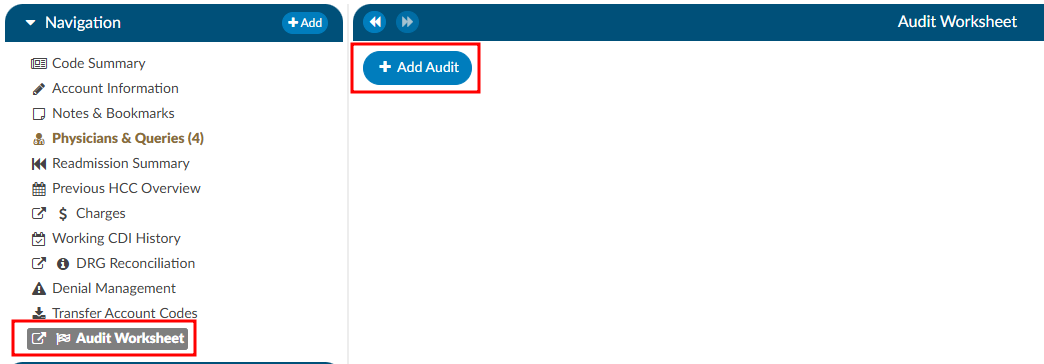
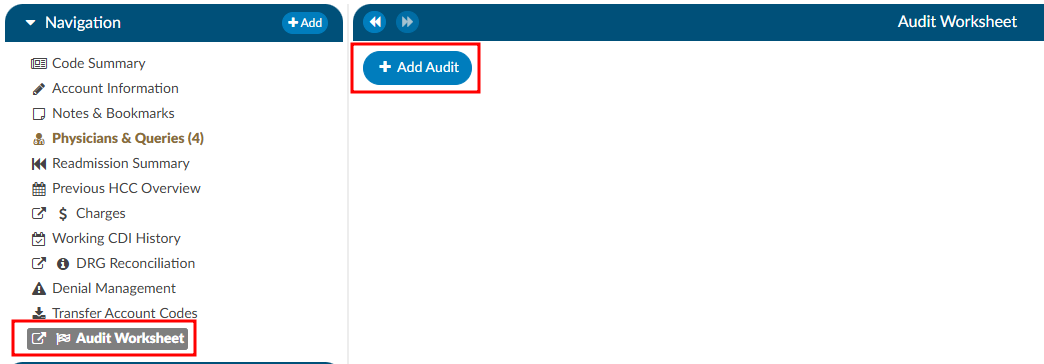
On the Navigation tree select the viewer called “Audit Worksheet”, then click the +Add Audit button to begin.
DRG Required
A DRG must be computed by a user before an audit can be started.
Step 4
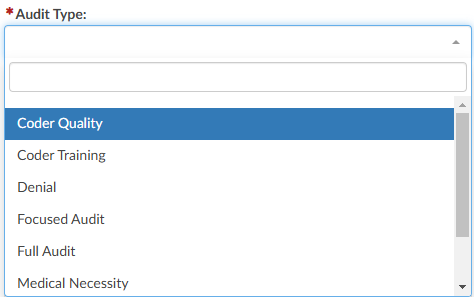
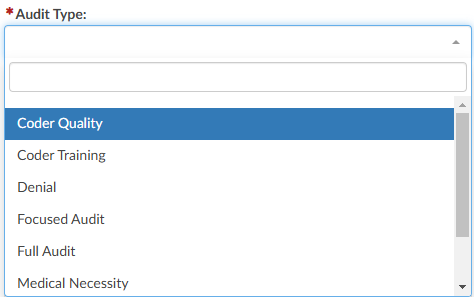
Select the appropriate audit type from the dropdown. This will be used for reporting on the types of audit performed and can also be used for workflow purposes. 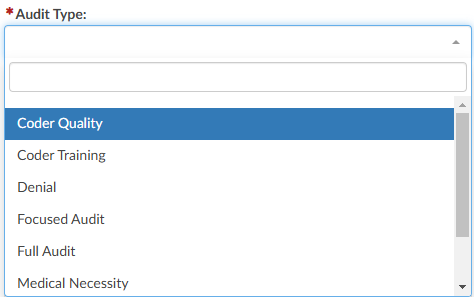
Step 5
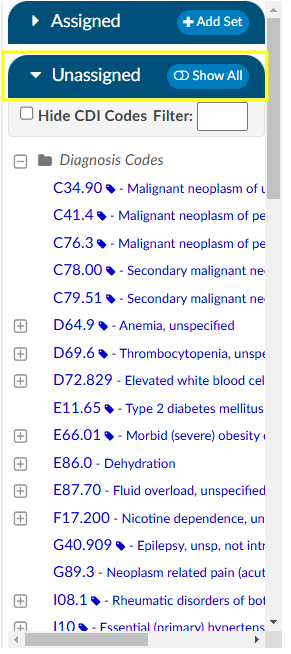
The codes in the Assigned code tree are the same codes initially submitted by the
Coder, allowing the Auditor to start the audit with the codes from the Coder. The Audit
viewer can be popped out onto a separate screen, allowing the Auditor to have a screen
for reviewing the chart. Selecting “Show All” codes in the Unassigned code tree and then clicking on the codes assigned, the
Auditor will load the documentation supporting that code. This will help streamline the audit process. 

Step 6
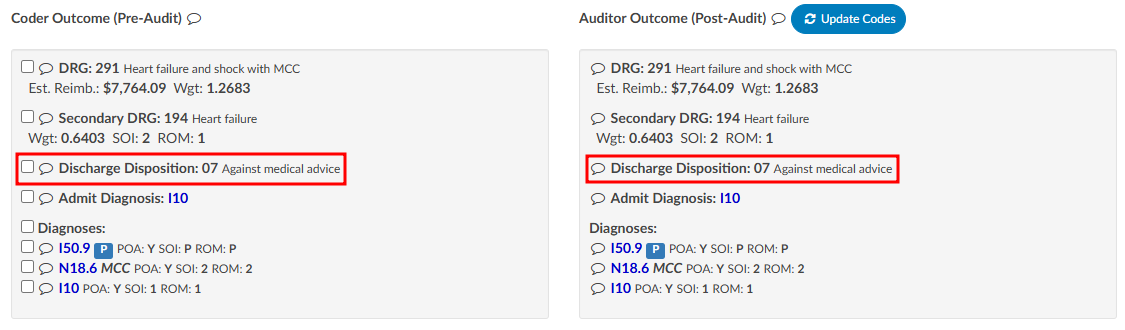
Once the Auditor has made changes and is completed with the audit, they can click “Update Codes”
which automatically calculates and populates the audit statistics section. There is a comment bubble
next to each code as well as the DRG for the Auditor to enter any comment(s). A symbol may display next to the codes.
- A green ‘plus’ sign will show if the code was added. 
 - A red ‘minus’ sign will show if a code was deleted.
- A red ‘minus’ sign will show if a code was deleted. 
 - A orange up or down ‘arrow’ sign will appear if the code location has been changed, as
in a primary and secondary are swapped.
- A orange up or down ‘arrow’ sign will appear if the code location has been changed, as
in a primary and secondary are swapped. 

Step 7
Although audit statistics have been automatically calculated and populated, the Auditor must
manually enter in the “Total Errors” which then automatically calculates the “Error Rate”.
Note
Because of its importance, and to include principal diagnosis changes in the error rate, changing the principal diagnosis counts as two errors intentionally.
- One error for changing a diagnosis code.
- A second error if the principal diagnosis is incorrect.
For an account with only two diagnosis codes, the error rate when the principal code is changed is 2 out of 3.
If on the same account the Auditor says the principal is correct and only changes the secondary code, the error rate is 1 out of 3.
Step 8
Complete additional sections as needed.
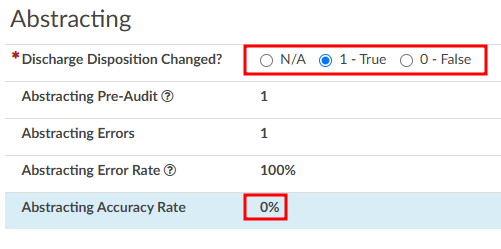
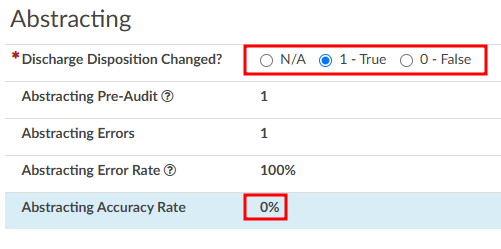
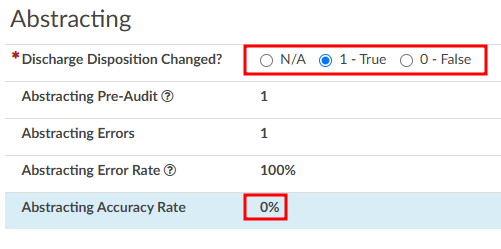
Abstracting
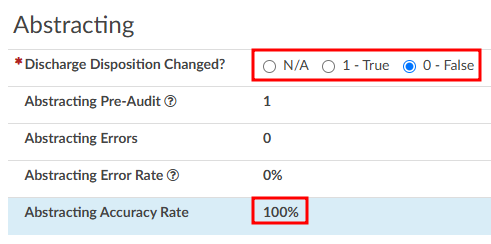
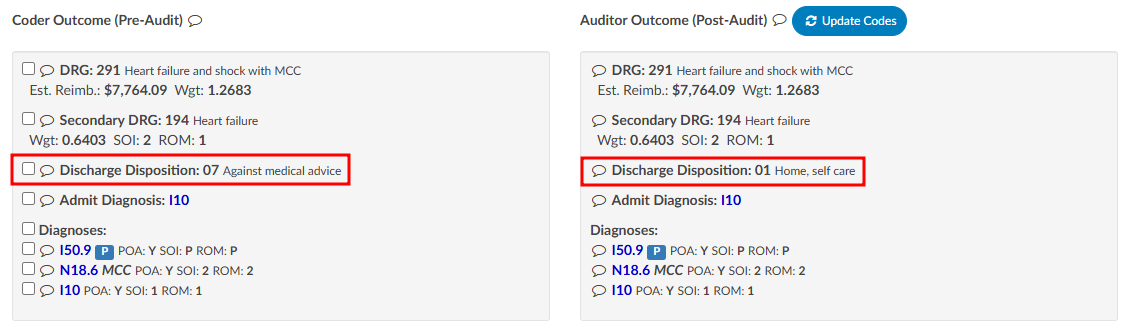
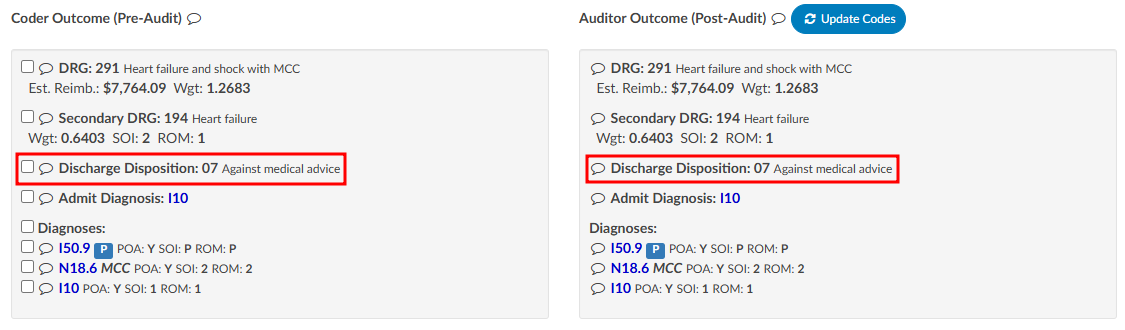
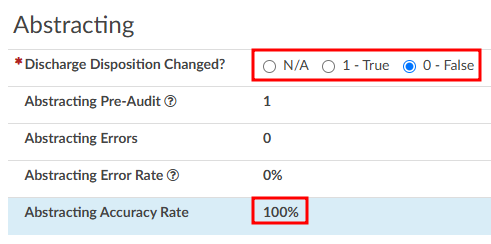
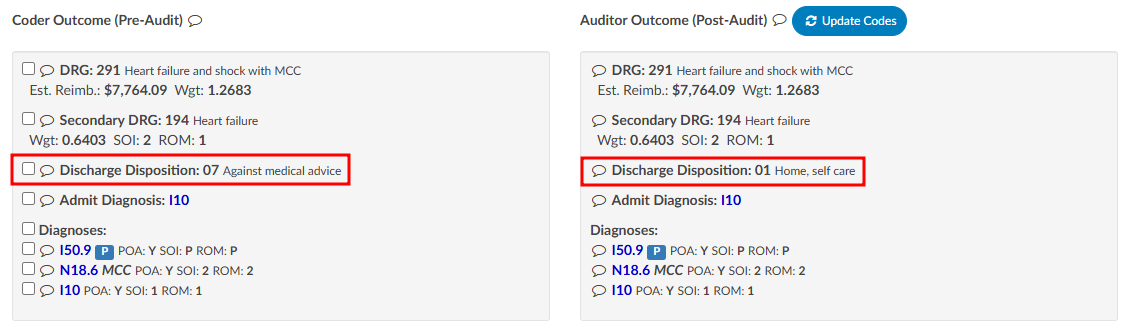
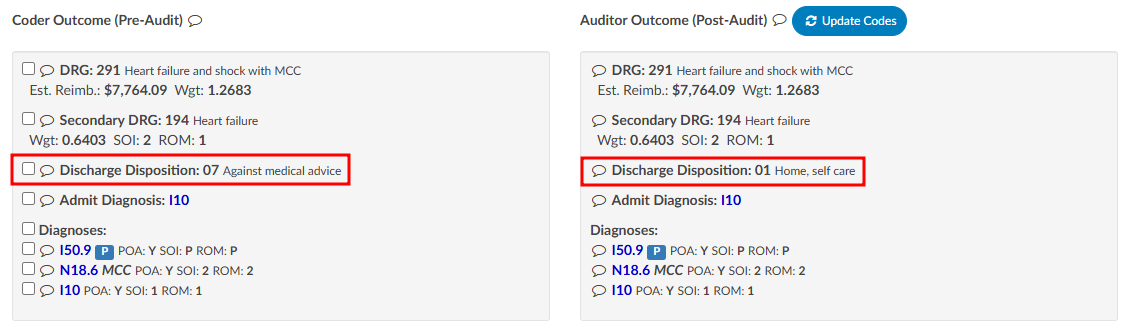
The Audit viewer also allows Auditors to review the abstraction performed by the Coder. Abstraction is managed on the Account Information page, and the specific fields audited can be customized. By default, the system audits the discharge disposition, but additional fields—such as point of origin, admit type, admit source, or others can be included upon request. To enable auditing for additional fields, contact the CAC Support Team (CACsupport@dolbey.com).
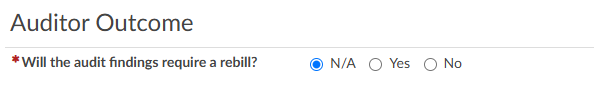
Once the desired fields are configured, the Auditor can make any necessary corrections directly in the Account Information viewer. Click on the Update Codes buttong next to the Auditor Outcome. This will cause the system to compare the updated information against the Coder’s original entries and include the selected Account Information fields for auditing.
Before:
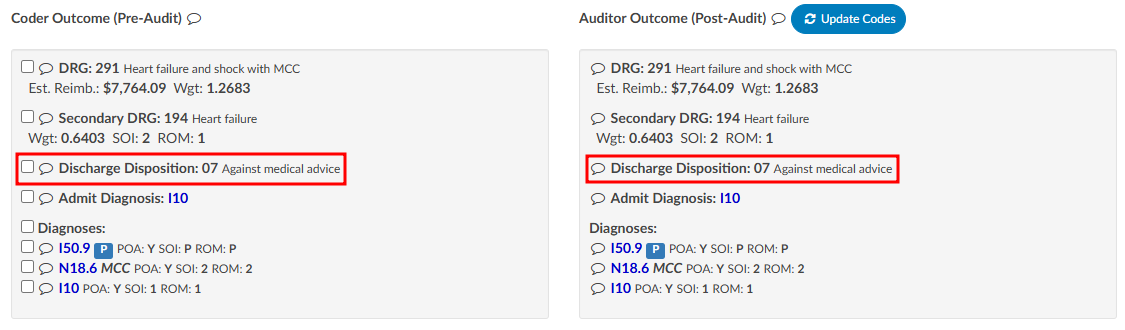
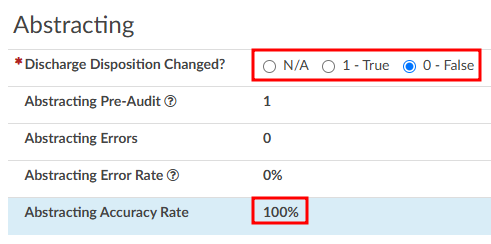
After:
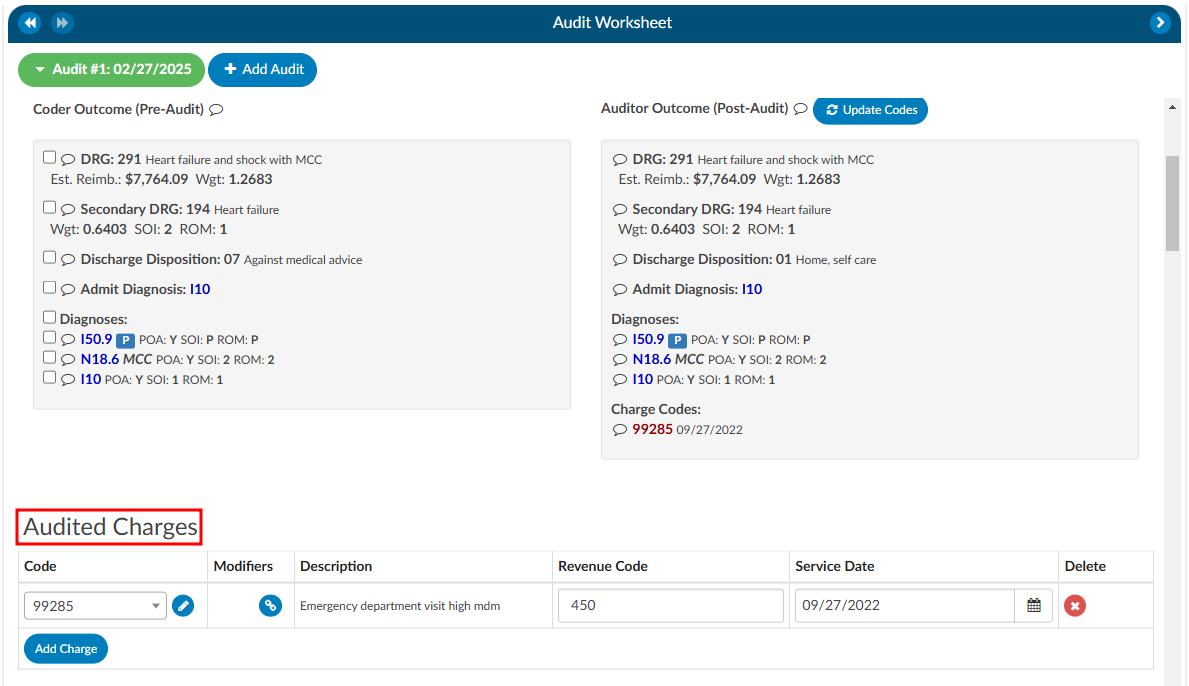
Charges
The Audit viewer also enables users to audit hard charges, but this functionality requires a configuration change by the CAC Support Team. To enable this capability, provide the CAC Support Team with the specific revenue codes to audit, as not all charges in the Charges or Transaction viewer will require auditing. Commonly audited revenue codes include 450 and 762, but others may apply depending on organizational needs.
Once the specified revenue codes are provided and configured, the Audit viewer will flag accounts containing charges that match the selected codes. When an audit is initiated, the user will see sections for “Charge Codes” listed under both the Coder Outcome and Auditor Outcome. Below these outcomes there will be a section for “Audited Charges,” where changes amde to the charges can be recorded.
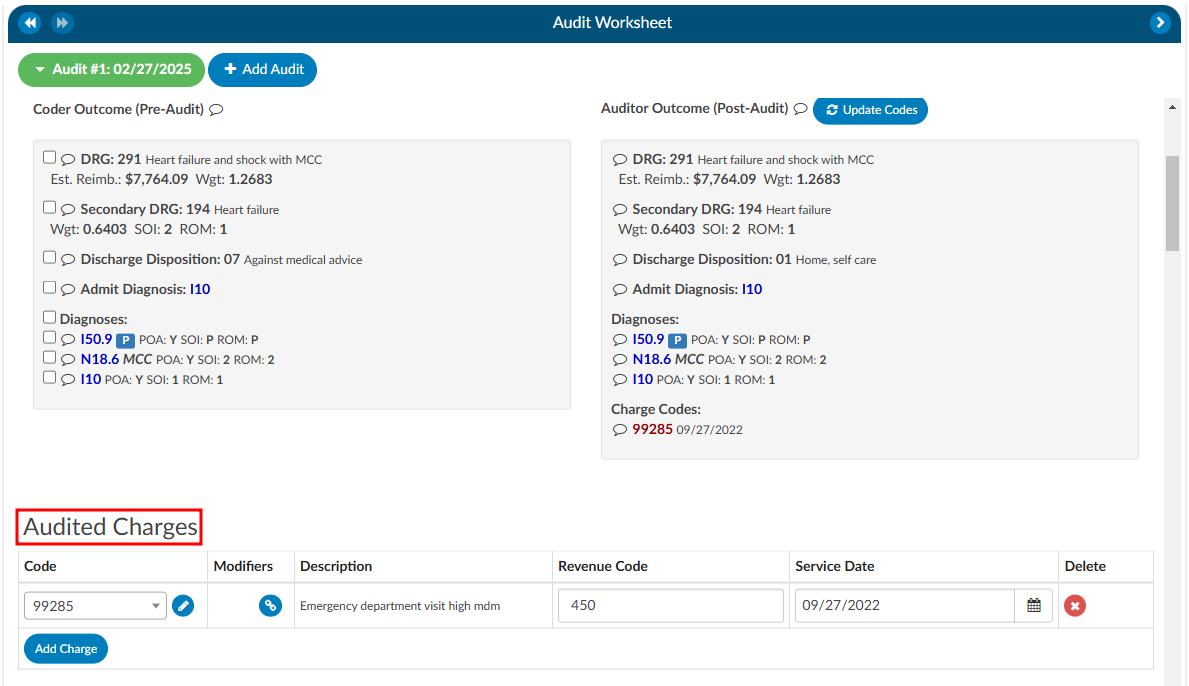
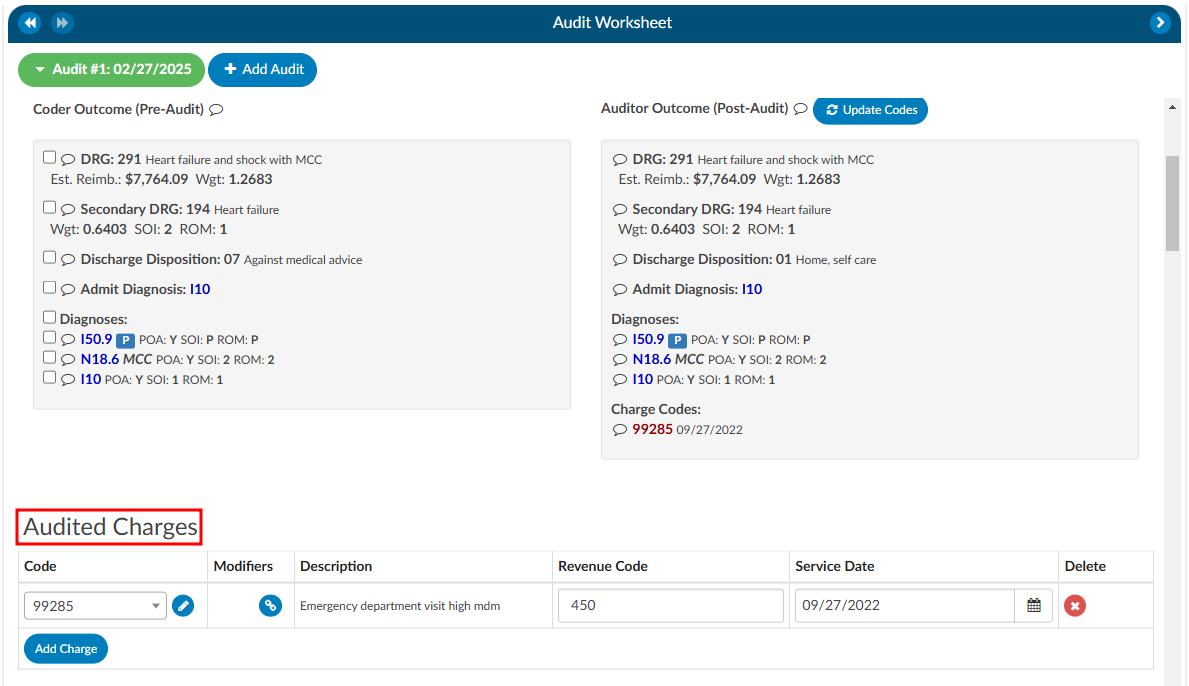
Updated Charges
It is important to note that most interfaces do not allow updated charges to be sent outbound. Therefore, the Auditor must manually record any changes on the audit worksheet. Changes can be made by directly editing the field or clicking the pencil icon, which launches the encoder, allowing the Auditor to look up CPT codes. The Auditor can also add modifiers, change the revenue code, or adjust the service date as needed.
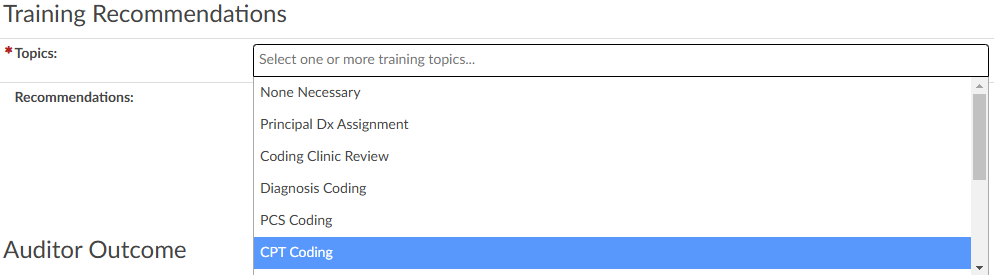
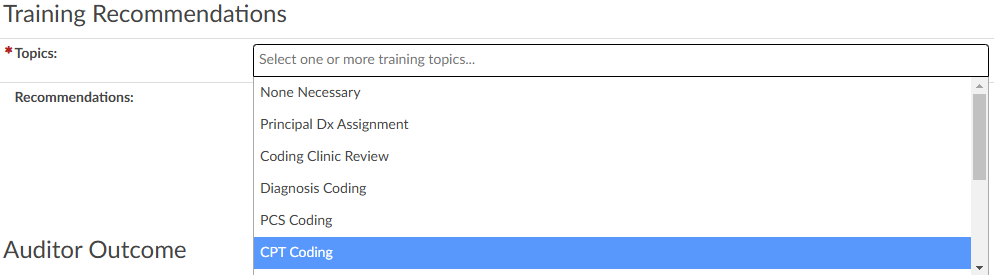
Training Recommendations
At the conclusion of the audit, the Auditor can list any recommended training topics. If no recommendations are necessary, “None” should be indicated. These topics can be modified using the mapping table. Additionally, the Auditor has space to provide any additional details as needed.
Auditor Outcome
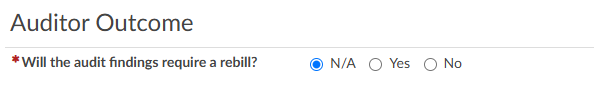
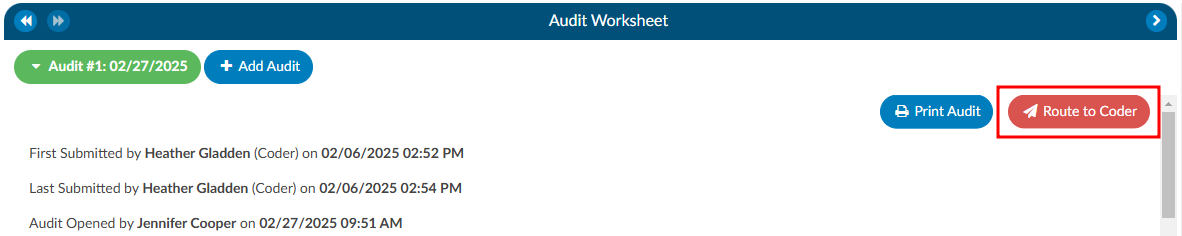
Step 9
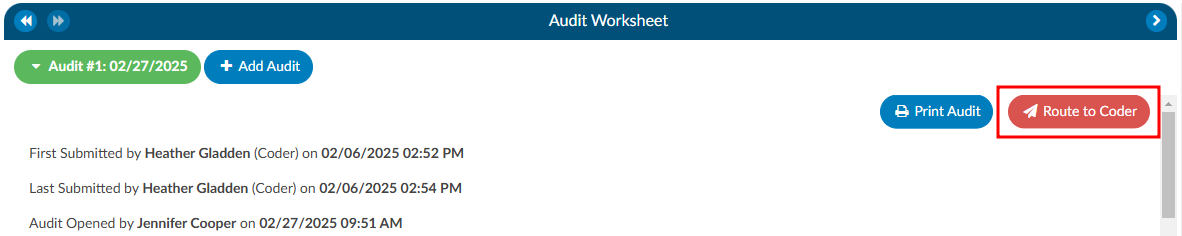
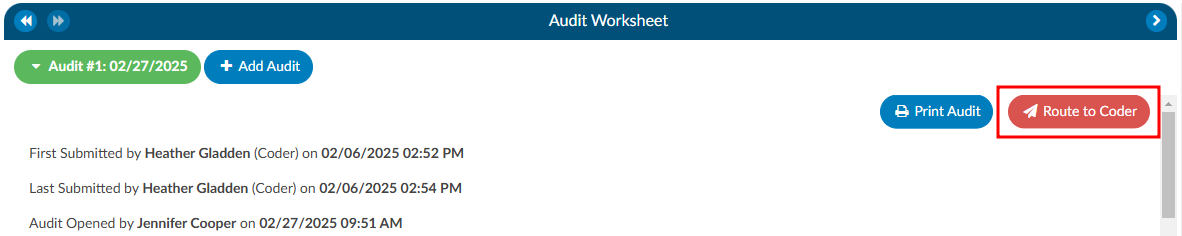
The Auditor can then re-submit the chart or route it back to the Coder of Record by using the
Route to Coder button in the top right corner of the audit worksheet. This will route the chart to
the Coder’s You worklist for the Coder to complete the Coder Acknowledgement section.
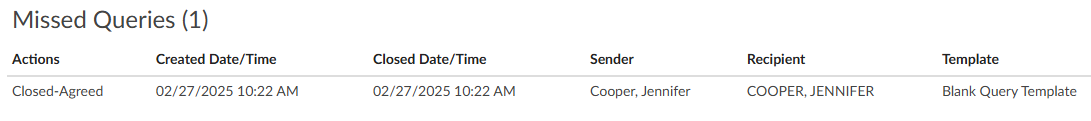
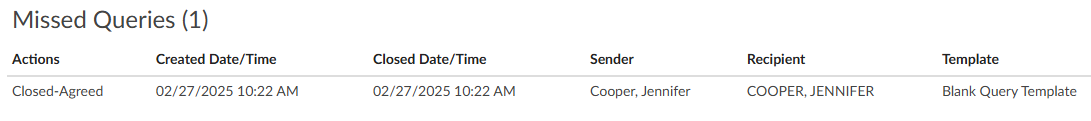
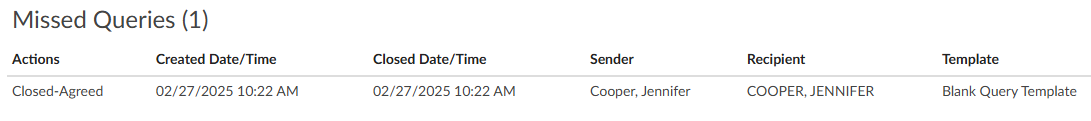
Missed Queries
This section will only be available if queries were initiated after the audit began. The query does not have to be initiated by the Auditor to be attributed to the audit as a missed opportunity.
Multiple Audits per Account
An account can have one or more audits added to it. Clicking the +Add Audit button will create a new, blank audit worksheet. These worksheets are numbered and displayed at the top of the Audit viewer, along with a date stamp indicating when each worksheet was opened. The worksheet currently being viewed will be highlighted with a green background.
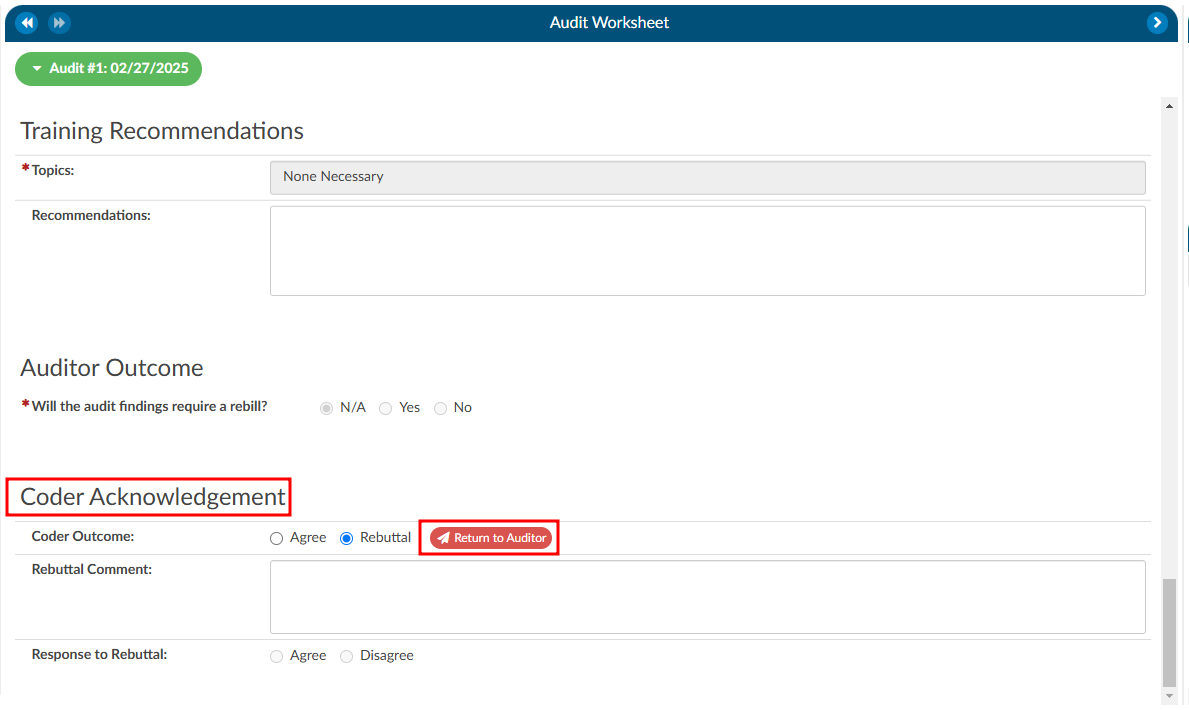
Coder Acknowledgement
If there are changes for the Coder to address post-audit, the Auditor will route the chart back to the Coder by clicking on the Route to Coder button.
When the Coder opens the chart to review, there will be a “Coder Acknowledgement” section. This section gives the Coder the opportunity to either agree with the audit or to provide a rebuttal. If the Coder selects the outcome to be a rebuttal the Coder must provide a comment for the Auditor. Once the Coder has added their comments they will route the chart back to the Auditor by clicking on the Return to Auditor button.
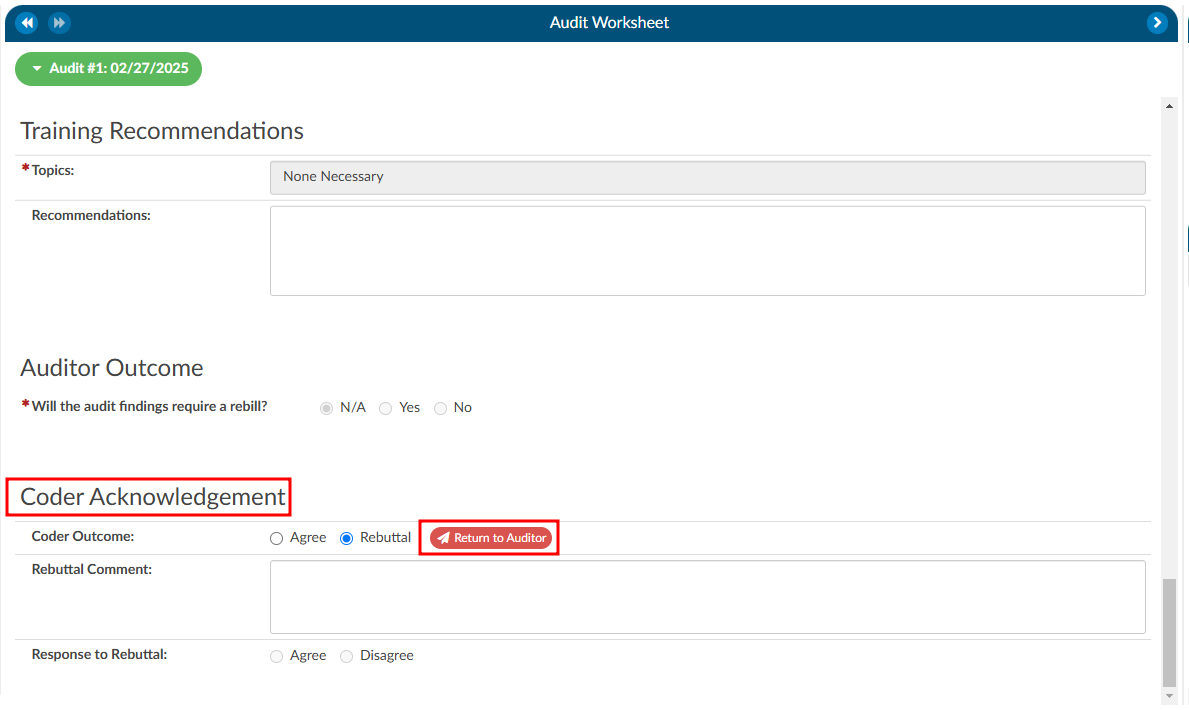
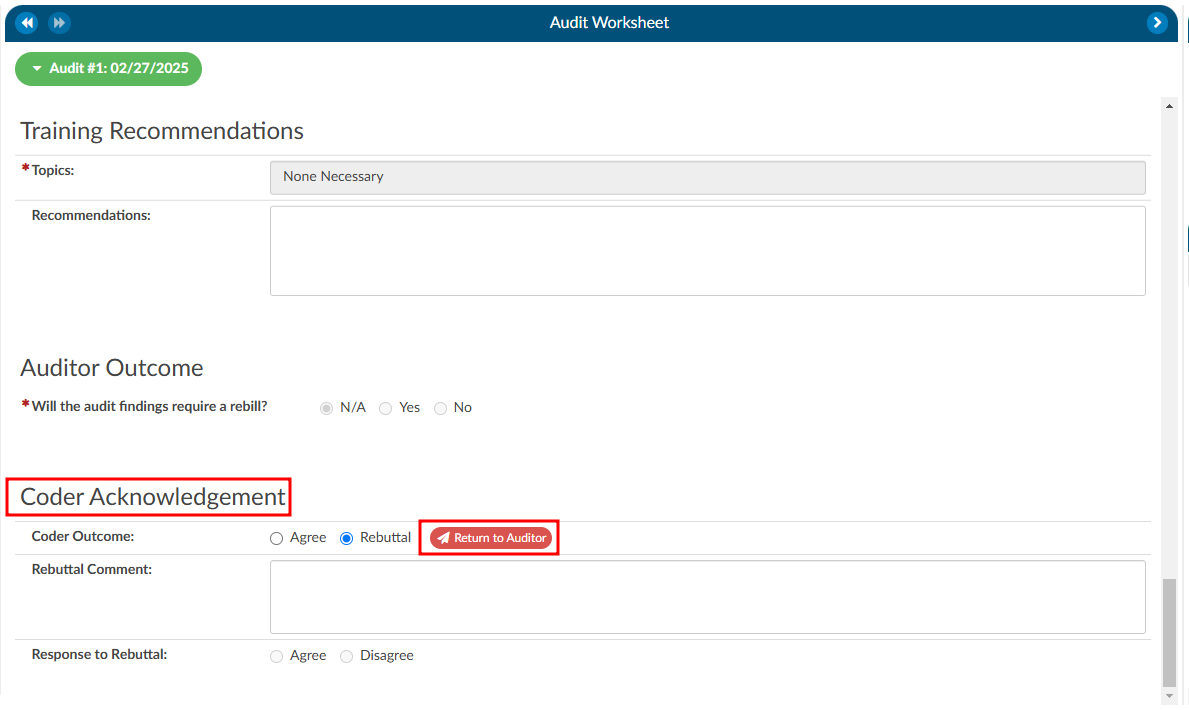
Once the chart is returned to the Auditor, there are a few actions the Auditor can take based on the Coder Acknowledgement response:
- Review the rebuttal, select agree, and finish the audit.
- Review the rebuttal, select disagree, and finish the audit OR initiate the Audit Escalation process.
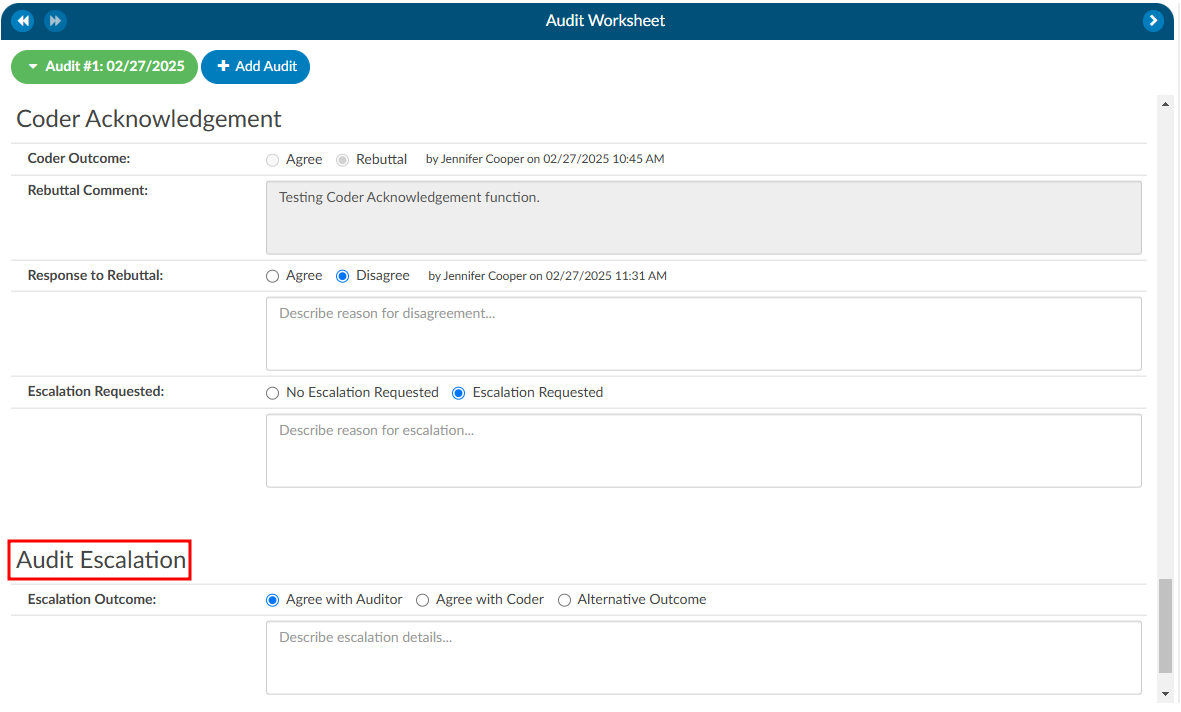
Audit Escalation
The Audit Escalation feature is triggered when the Coder’s outcome results in a rebuttal, and the Auditor disagrees with the rebuttal and further action may need to be taken. In this case, a section labeled “Escalation Requested” becomes available. The Auditor can activate this section to indicate that an escalation is necessary. Once this is set, an additional section called Audit Escalation will appear. This section allows the user to document the outcome of the escalation and provides a designated space for comments related to the escalation.
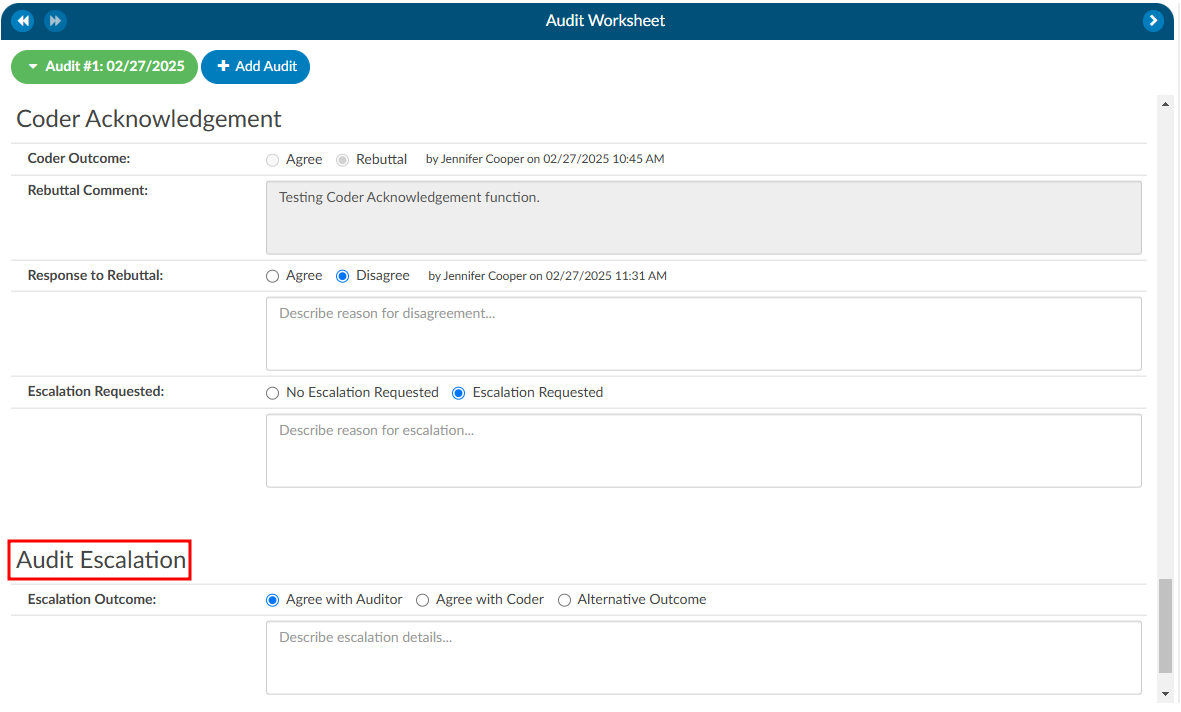
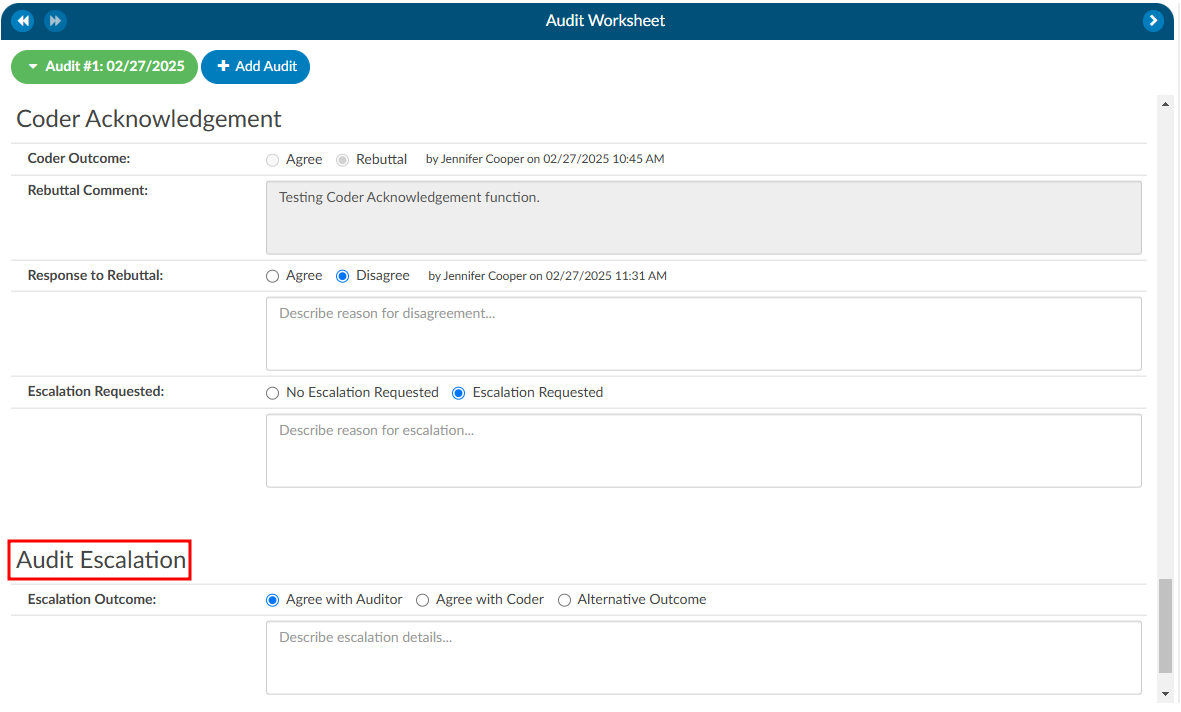
This feature is governed by role-based permissions in the Role Management settings. Within Role Management, there is an option to specify who has the ability to edit the Audit Escalation section.
If a coding manager or another designated individual is responsible for responding to escalations, they must meet the following requirements:
- Audit View Access: The user’s role must include permissions to view audits.
- Audit Role Setting: The role assigned to the user must have the Audit option enabled in the top-right corner of Role Management.
- Edit Escalation Access: The user must also have explicit permission to edit escalations, as defined within the Role Management settings.
These permissions ensure that only authorized individuals can manage and resolve the escalation process effectively.s
Finishing an Audit
To finish an audit, whether it goes through a rebuttal process or not, the Auditor would simiply click on the Finish Audit button. This closes the audit, but the Auditor has the option to re-open the audit as needed.
Audit Statistics
Diagnosis Added: Codes added to the assigned codes list by quantity.
ex. If the coder has 5 total diagnosis codes and the auditor has 6 total diagnosis codes, the number of added codes is 1 (because the auditor added an additional code).
Diagnosis Codes Unassigned: Codes removed from the assigned codes list by quantity.
ex. If the coder has 5 total diagnosis codes and the auditor has 3 total diagnosis codes, the number of unassigned codes is 2 (because the auditor removed two codes).
Diagnosis Codes Edited: Codes that are different between the assigned code lists by comparing the auditor’s codes to the coder’s code, but not counting the number of codes added or unassigned.
ex. If a coder has 5 total diagnosis codes, and the auditor changed 2 of them without adding or unassigning codes, the number of edited codes is 2 (because the auditor “swapped out” two of the codes from the coder with different ones).
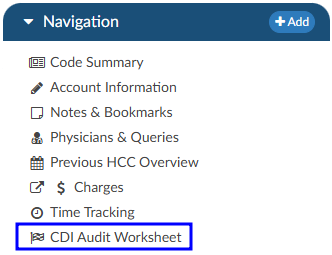
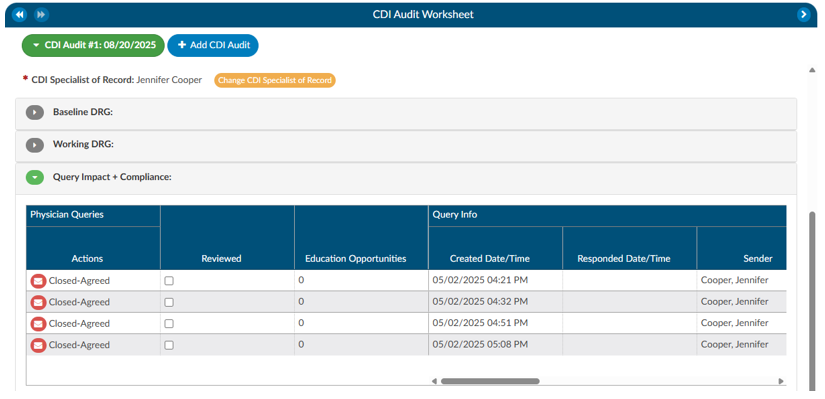
CDI Audit Worksheet
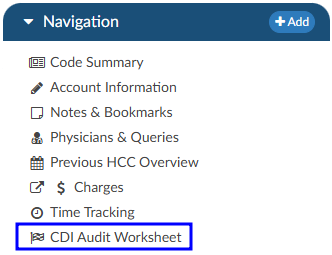
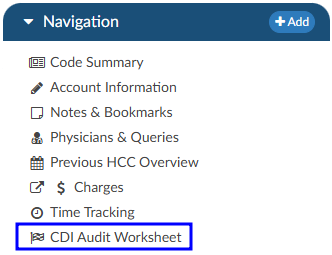
Starting a CDI Audit
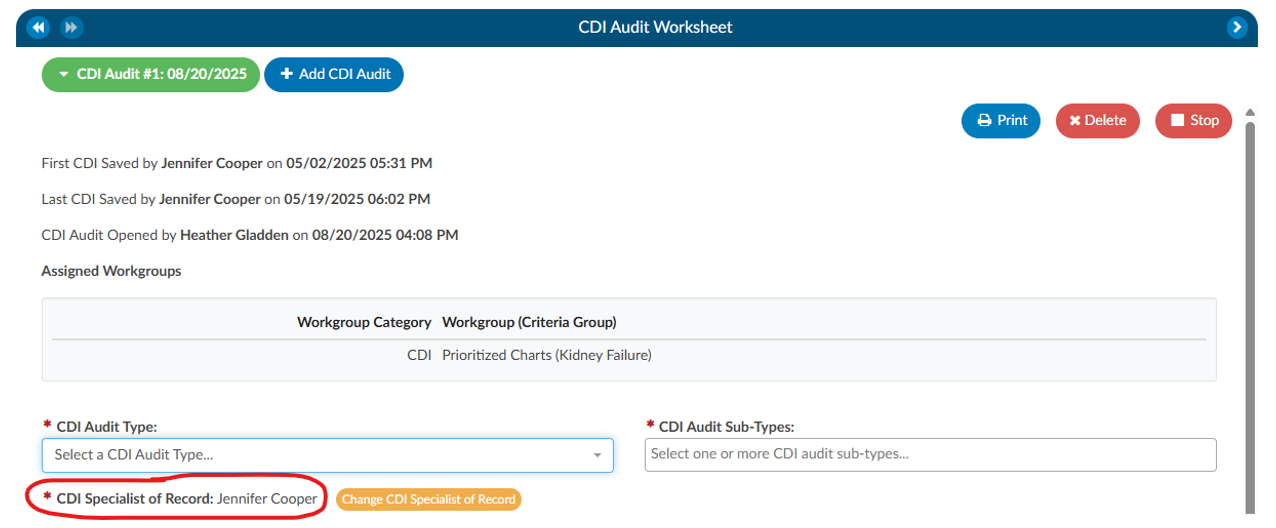
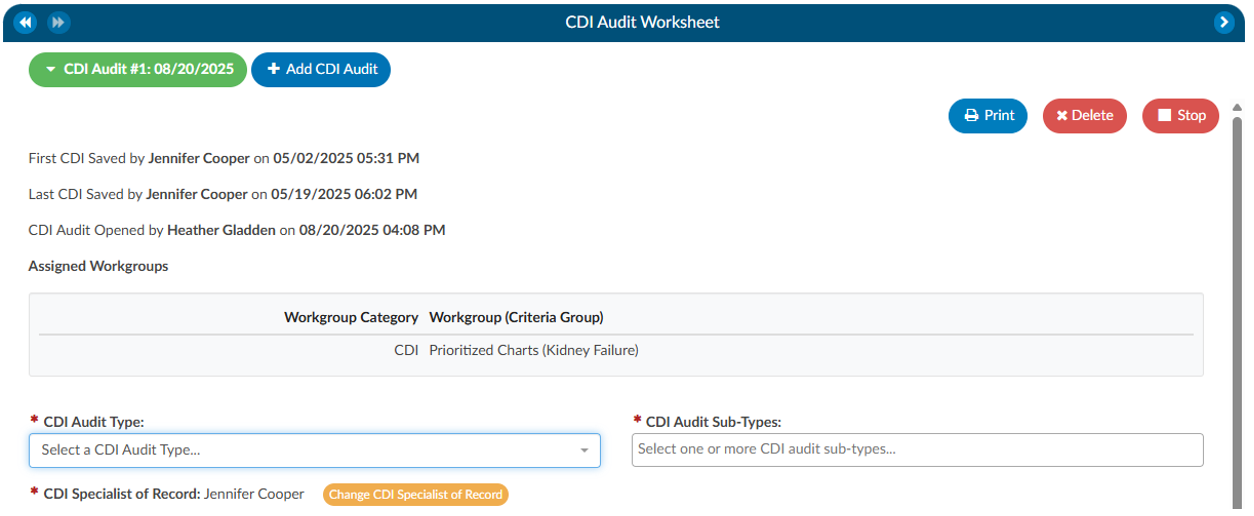
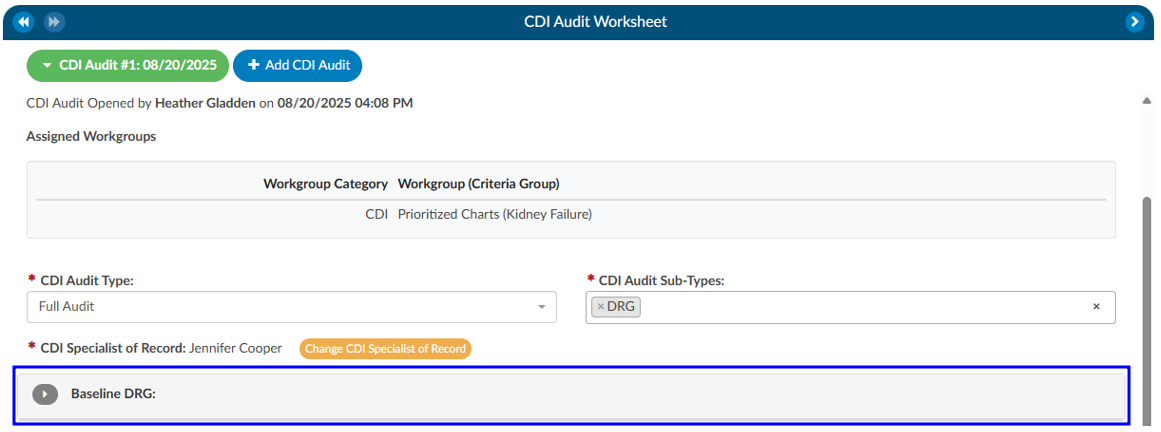
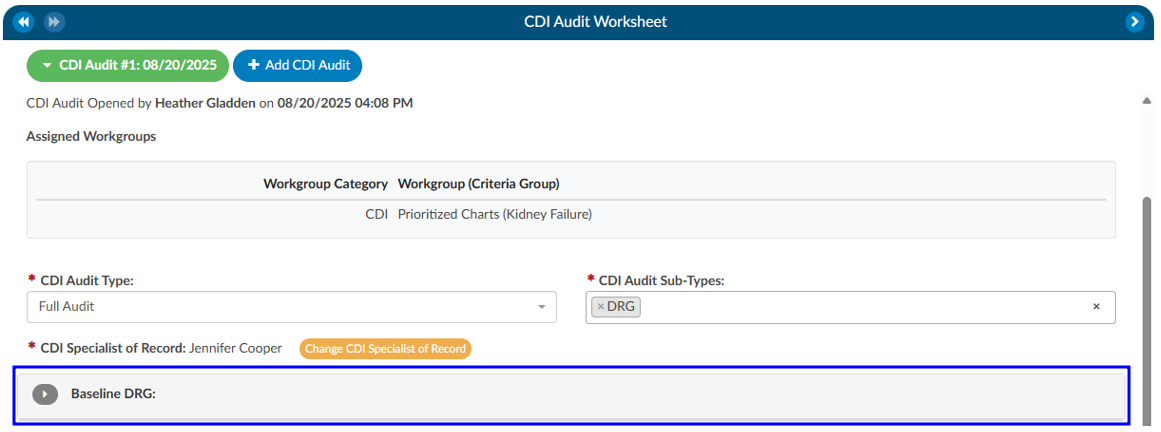
Once prerequisites are met, you can begin the audit process:
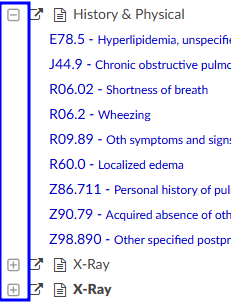
- Select a Patient Chart: Open a patient chart that includes a baseline DRG.
- Locate the CDI Audit Worksheet: Within the chart’s navigation tree, click on the CDI Audit Worksheet.
- Start the Audit: Select Start Audit to launch the audit session.
At this point, the audit is only visible to a limited group of users. These include:
- The CDI of record, who is the primary subject of the audit.
- Other CDI auditors, who have authority to perform or review audits.
- System administrators, who maintain oversight.
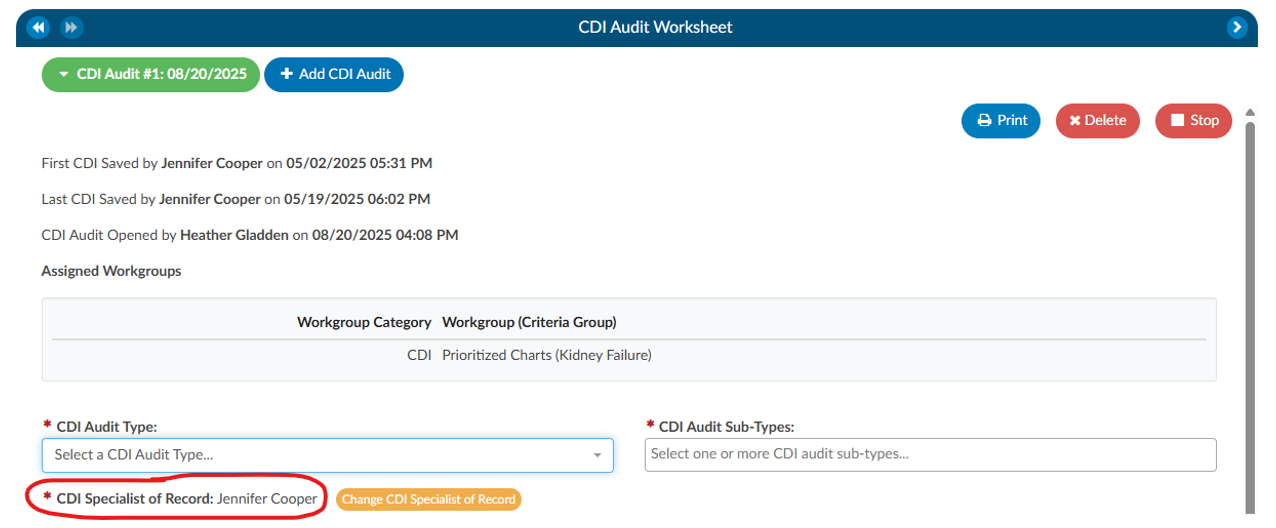
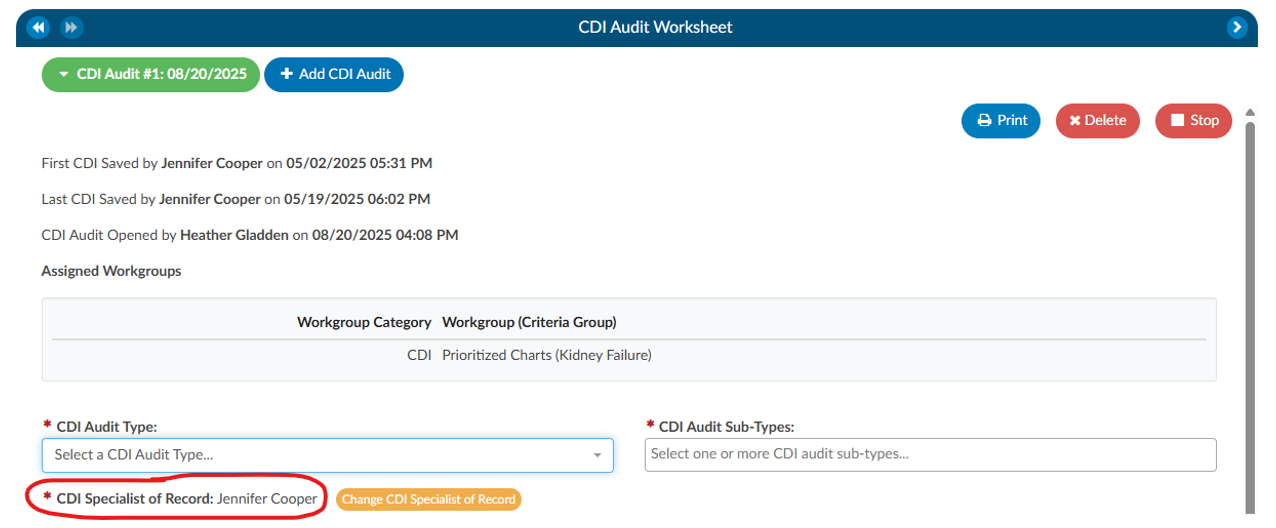
The audit displays the CDI Specialist of Record, showing which CDI user is being evaluated. If you need to audit a different CDI user, you may select their name from the drop-down menu. This is especially important in cases where more than one CDI professional has worked on the same chart.
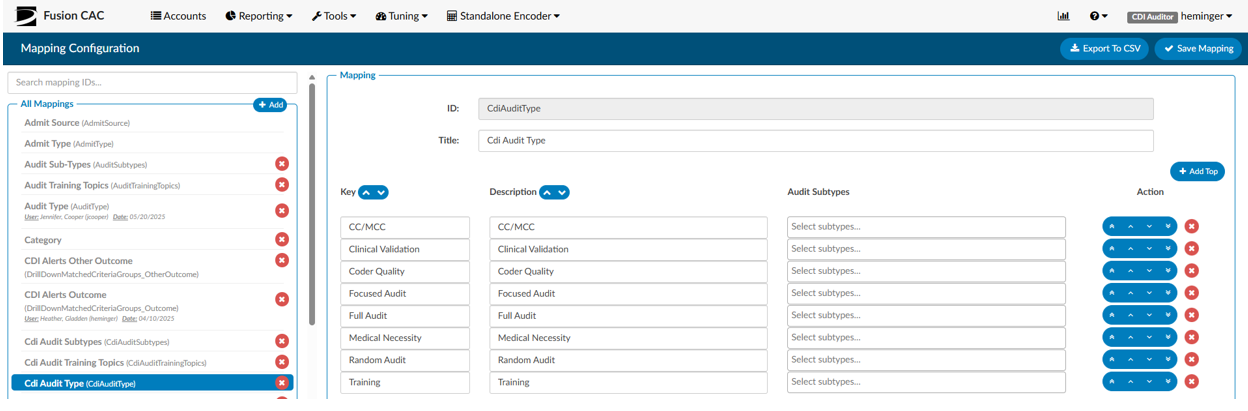
Selecting Audit Types and Subtypes
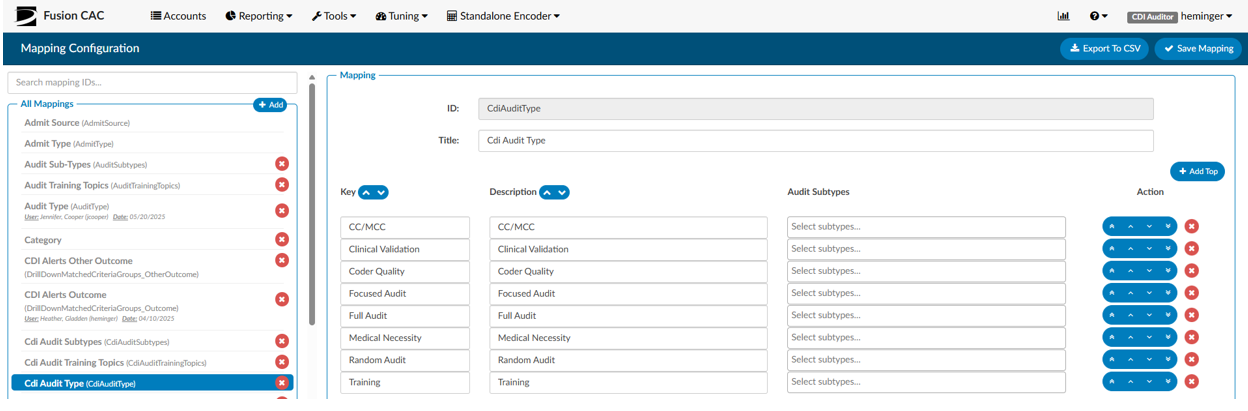
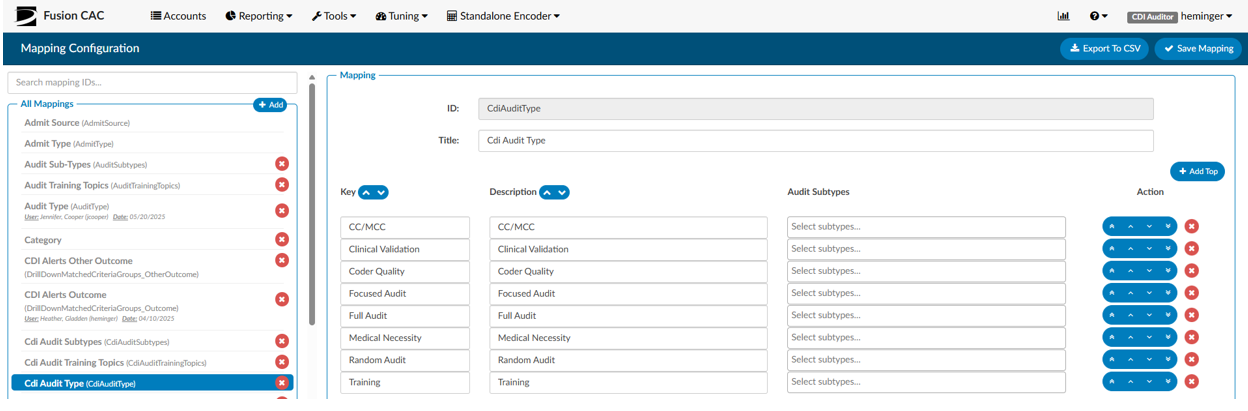
When beginning an audit, you are required to choose an audit type. This classification is used for reporting and allows leadership to track and analyze the kinds of audits being performed.
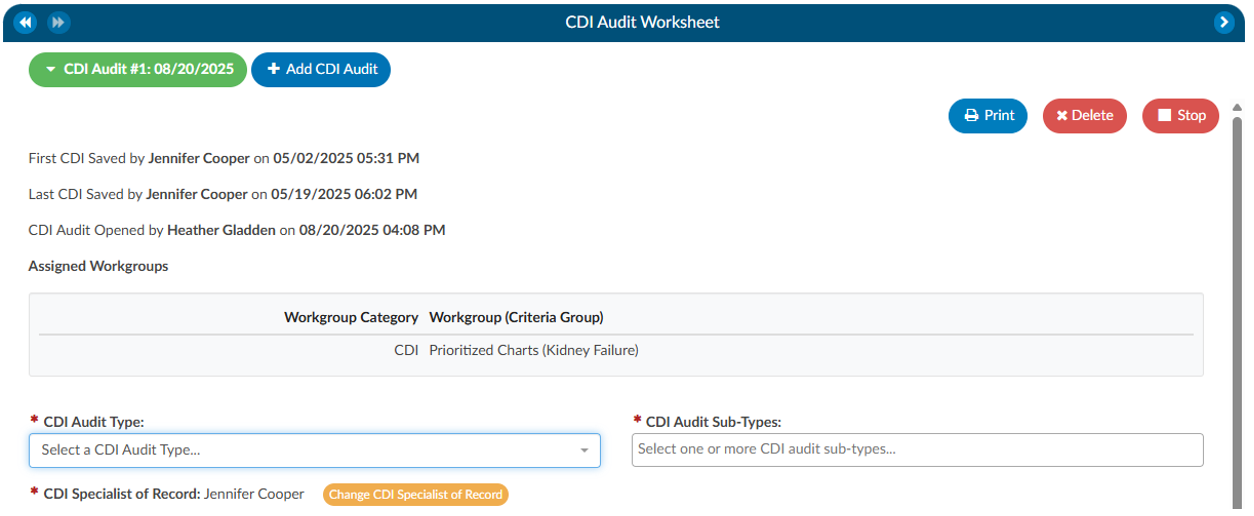
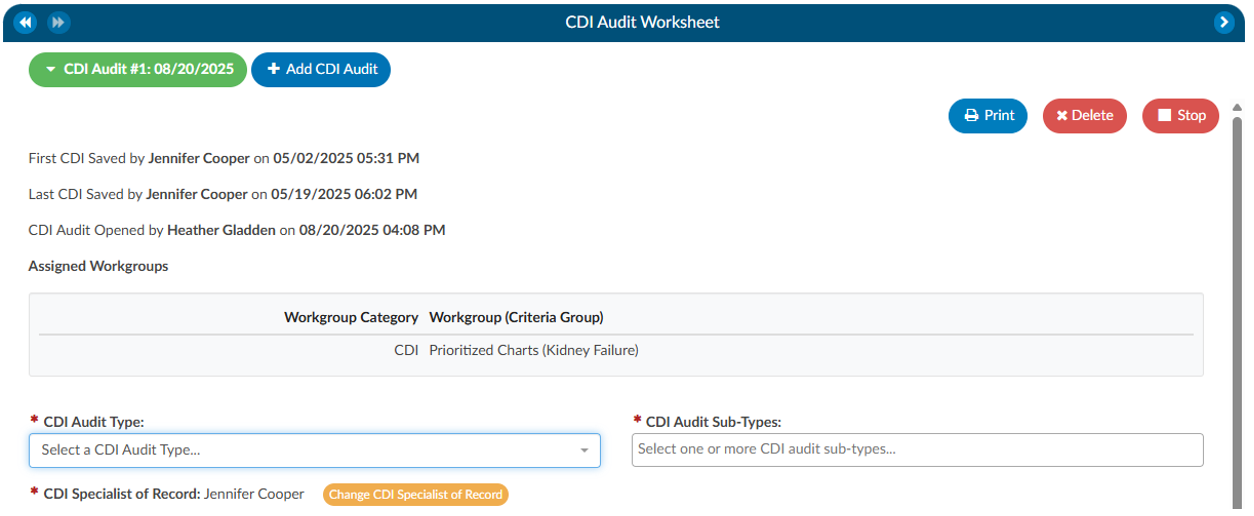
Audit types can be customized within the system by navigating to Tools → Mapping → CDI Audit Types. In addition to the audit type, you can also assign one or more audit subtypes. Subtypes allow you to specify the focus of the audit. For instance, if the purpose is to evaluate a trainee’s performance, you might choose “CDI User in Training” as a subtype. If the goal is to validate whether the baseline DRG was appropriately assigned, you could select “Baseline DRG Review.” Subtypes may be tied to specific audit types and can be customized by your organization. This classification ensures that reporting can reflect both the general purpose of the audit and its specific focus.
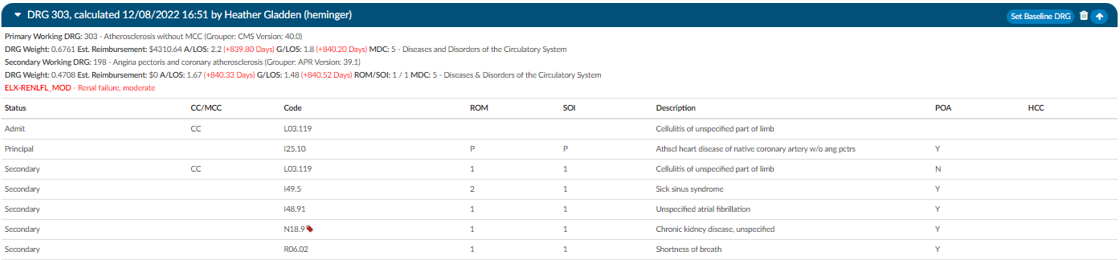
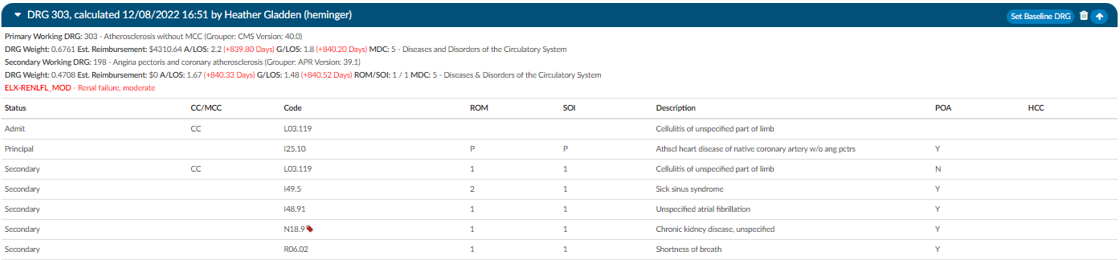
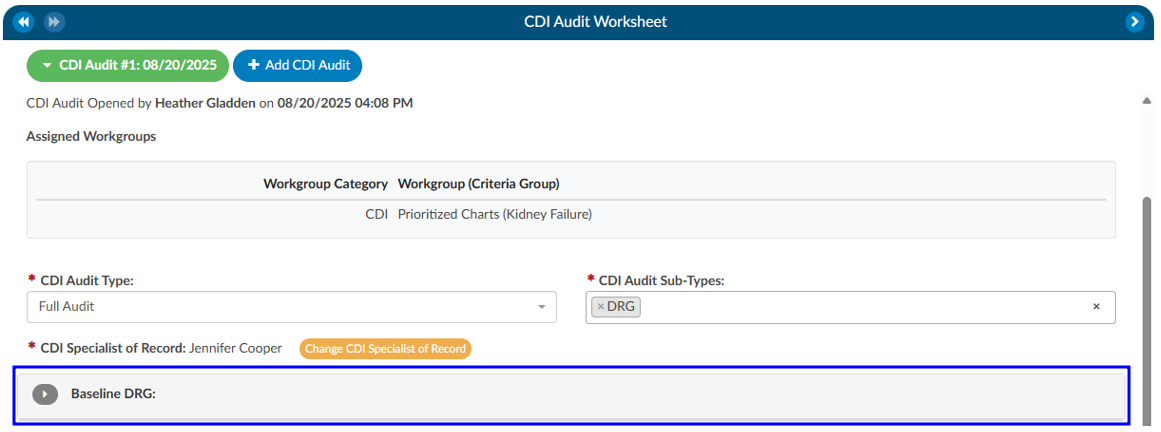
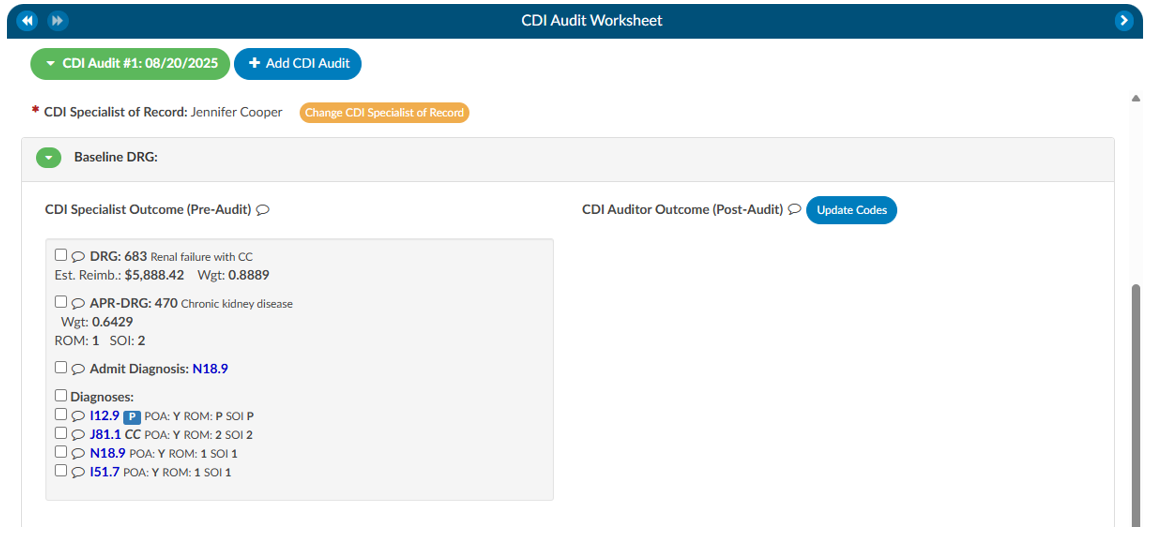
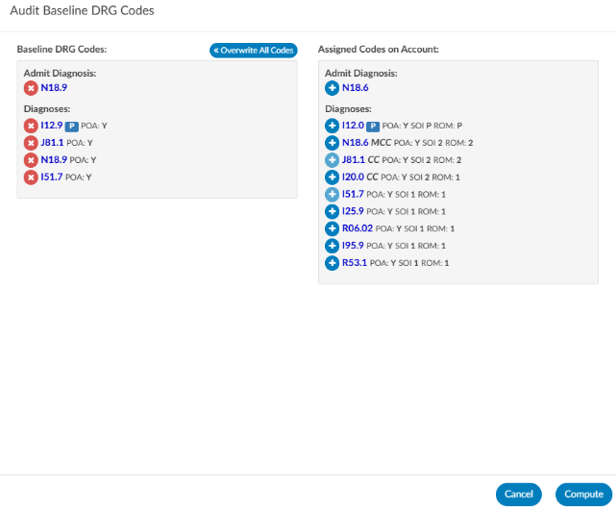
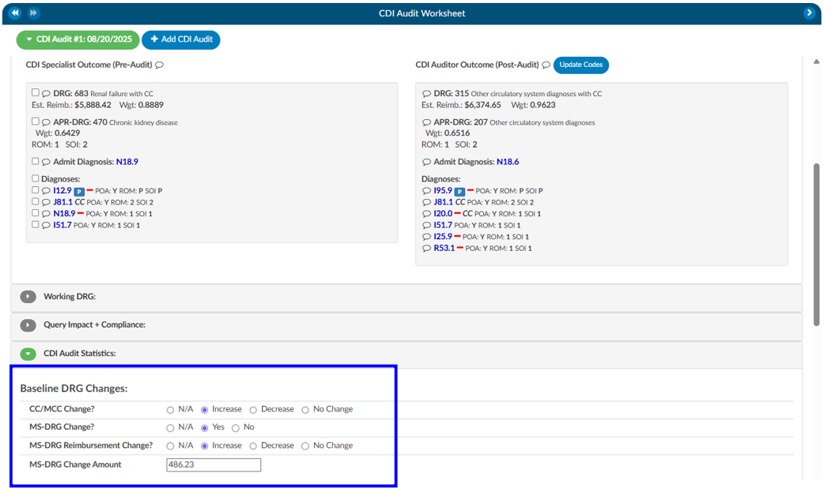
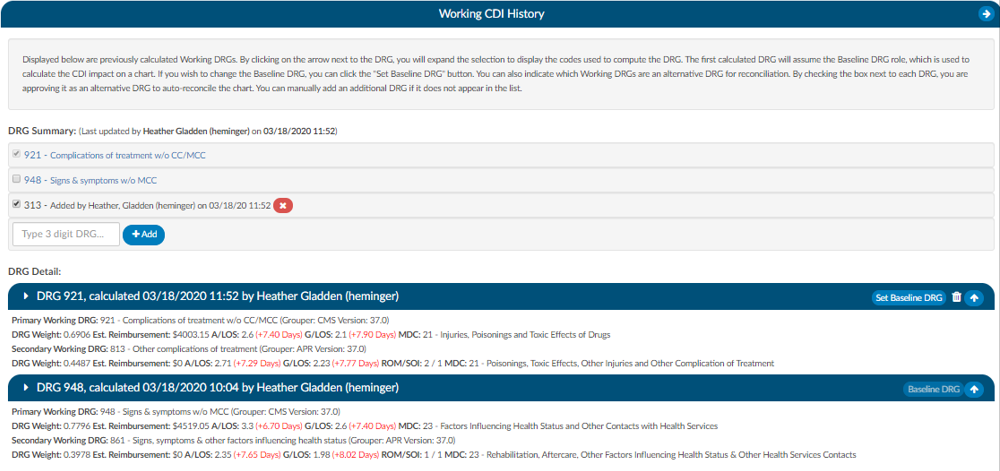
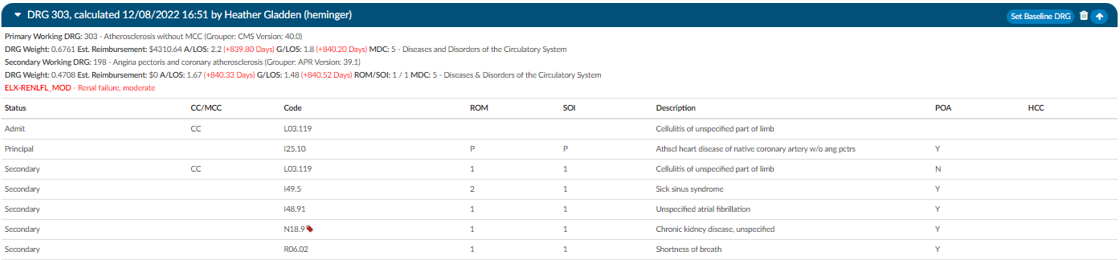
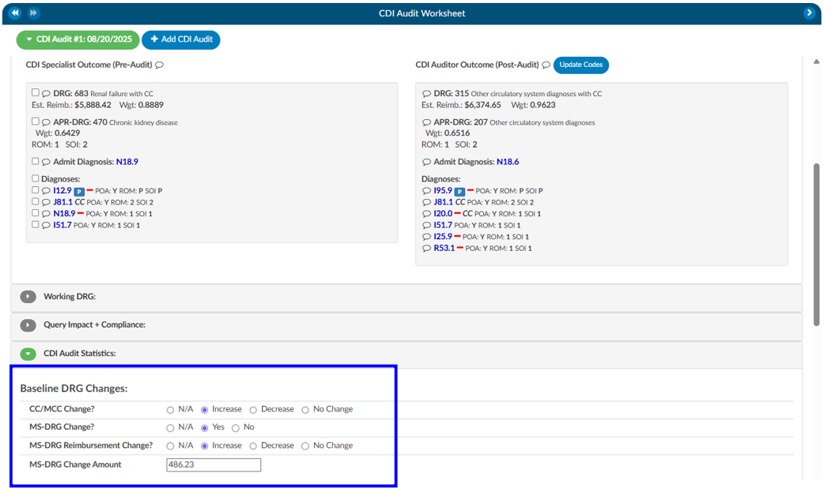
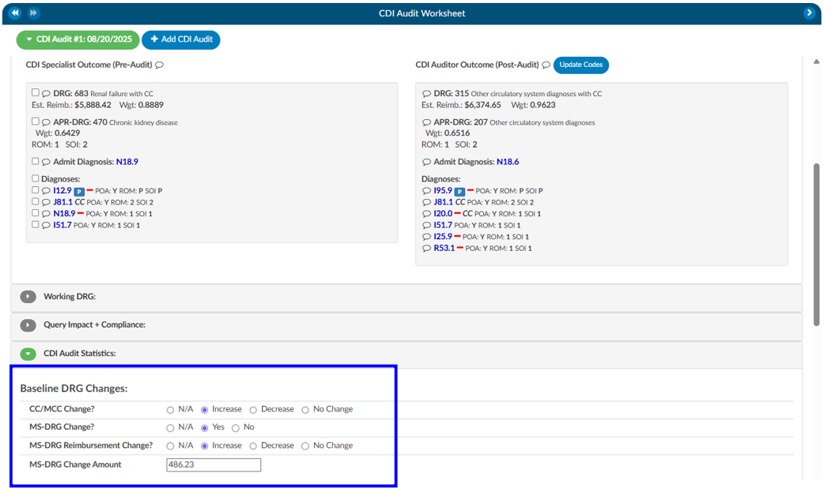
Reviewing the Baseline DRG
The first major step in the audit is evaluating the baseline DRG assigned by the CDI of record.
- Expand the Baseline DRG Section: By default, this section is collapsed. Expanding it reveals the baseline DRG chosen by the CDI.
- CDI Specialist Outcome: This is the Baseline DRG and the codes that went into the Basline.
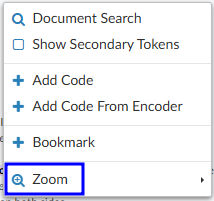
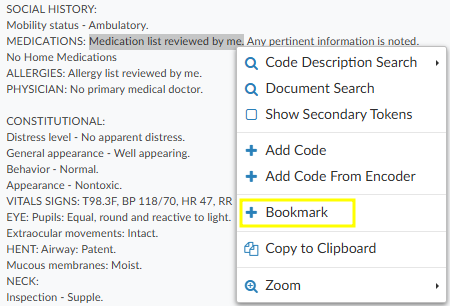
- CDI Specialist Outcome: This is the Baseline DRG and the codes that went into the Basline.
- Adding Missing Codes:
- If the necessary code does not appear on the right-hand side, you can minimize the editor by clicking the red button in the top-right corner.
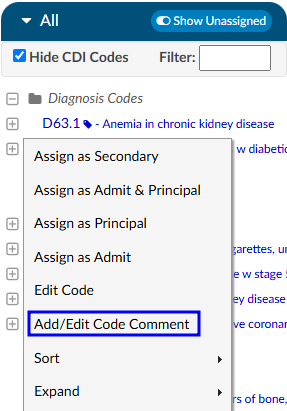
- From there, you can find the appropriate documentation or unassigned codes. Right-click to either Add Code or Add Code from Encoder.
- After adding the code, reopen the editor, move the code into the baseline DRG list, and save.
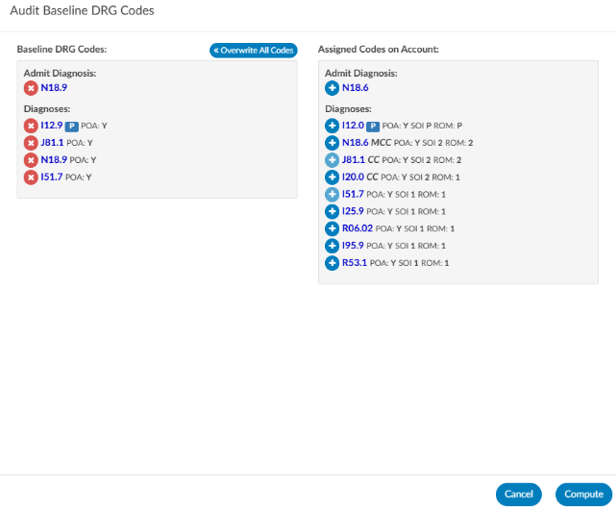
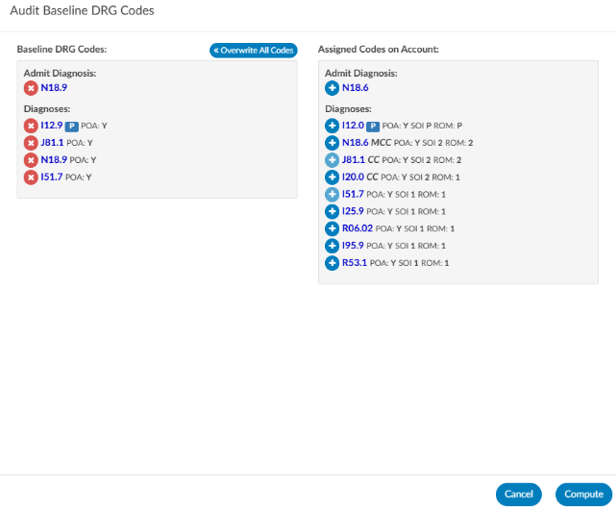
- Update Codes: If the CDI wants to change the existing CDI DRG they will need to add codes if not already in assigned code tree. Then click on Update Codes to open the coding editor.
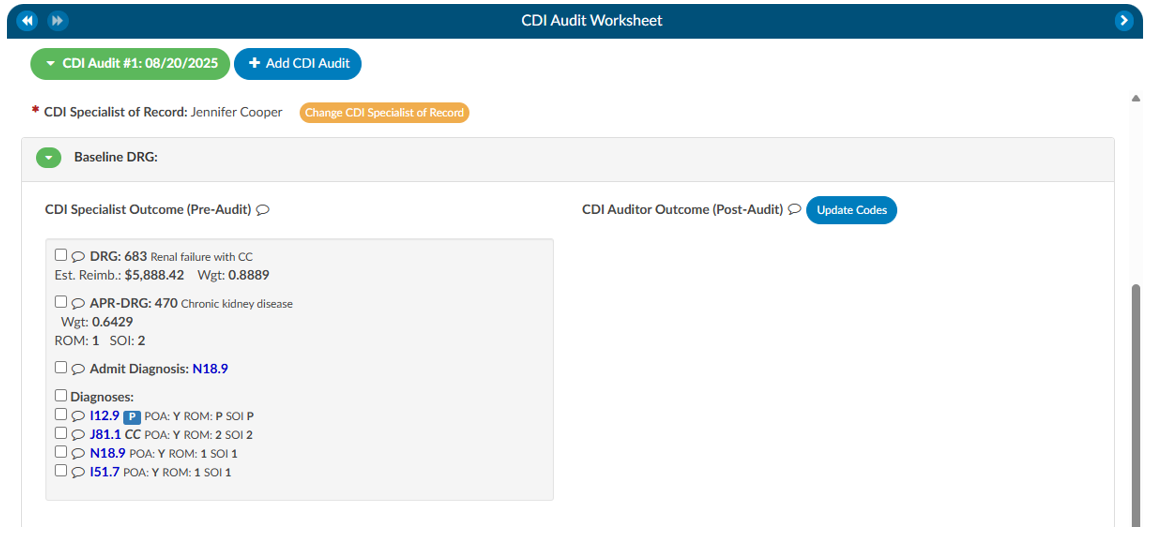
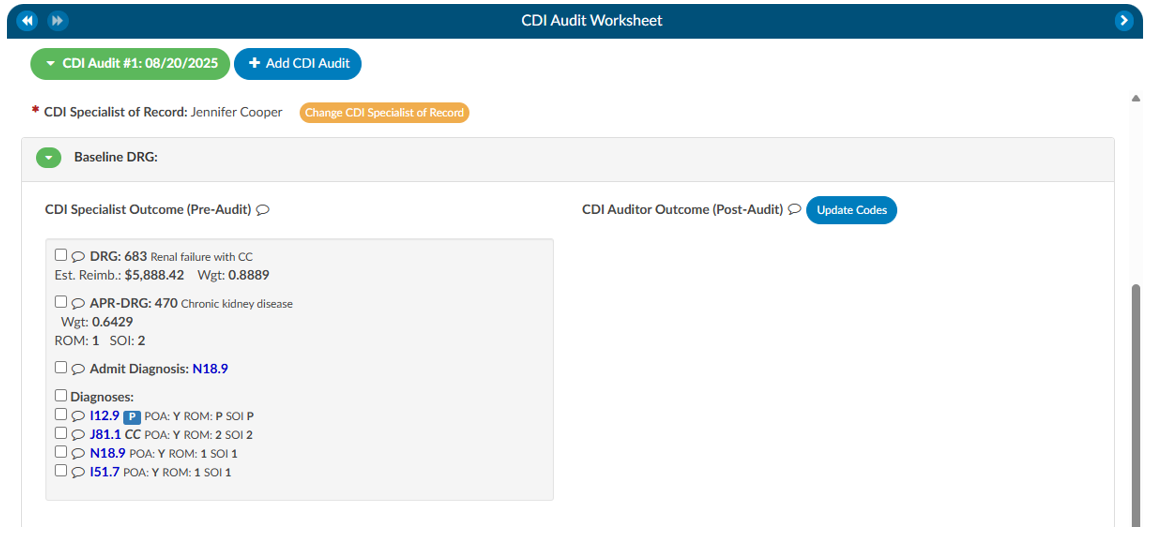
- Editor Presents two Panels:
- Left side: Displays the codes used to calculate the current baseline DRG.
- Right side: Displays the system’s assigned code tree, showing all available codes. Move any codes from the right to the left if you want the audited Baseline to use these codes.
Reviewing the Working DRG
After validating the baseline DRG, the next step is to review the working DRG. This process is nearly identical to the baseline review. By expanding the working DRG section and selecting Update Codes, you can access the editor, compare codes, and make adjustments as necessary. The working DRG reflects the CDI’s evolving assessment of the case and is often compared against the baseline DRG for consistency and accuracy.
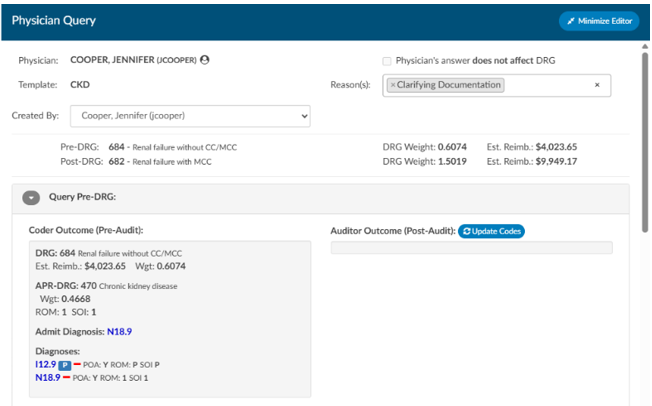
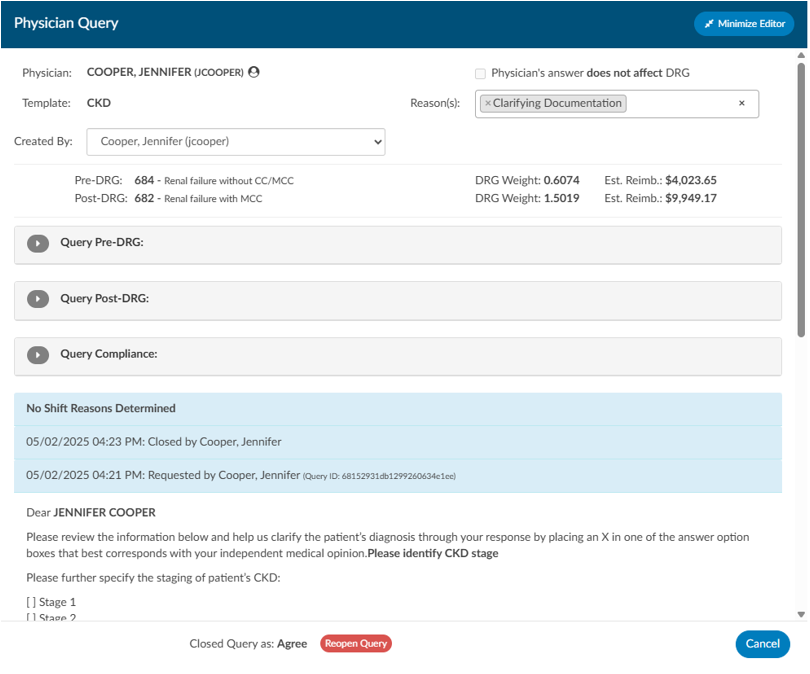
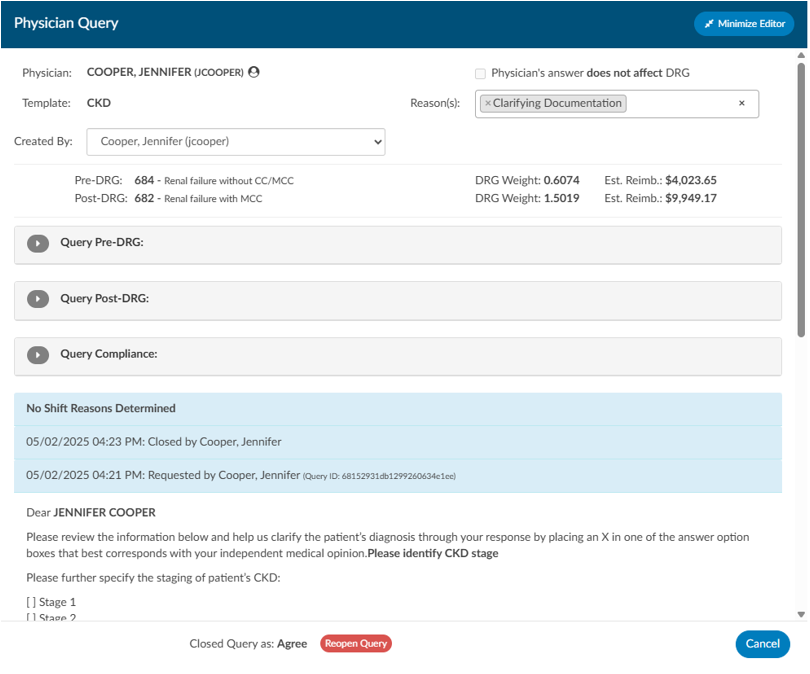
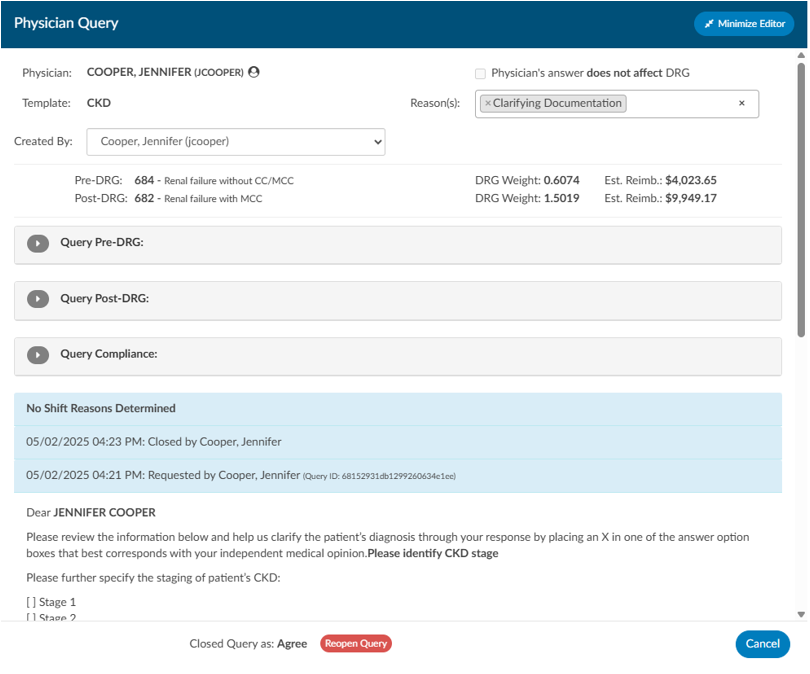
Query Compliance Review
The third key component of the audit involves query compliance. If queries were issued by the CDI of record, you will see them listed under the Query Statistics section. If no queries were created, this section will not appear.
It is important to note that the module only displays queries created by the CDI user listed as the owner of the audit. If another CDI professional also issued queries on the chart, you must start a separate audit under that individual’s name to review their work.
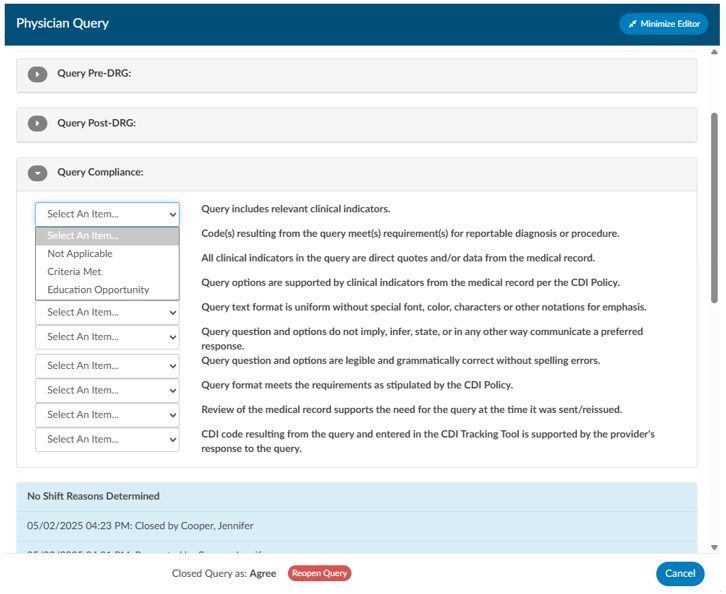
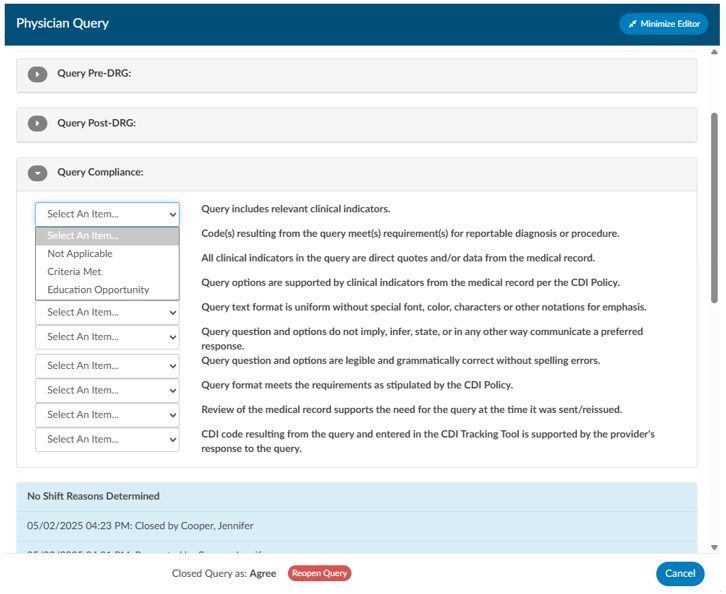
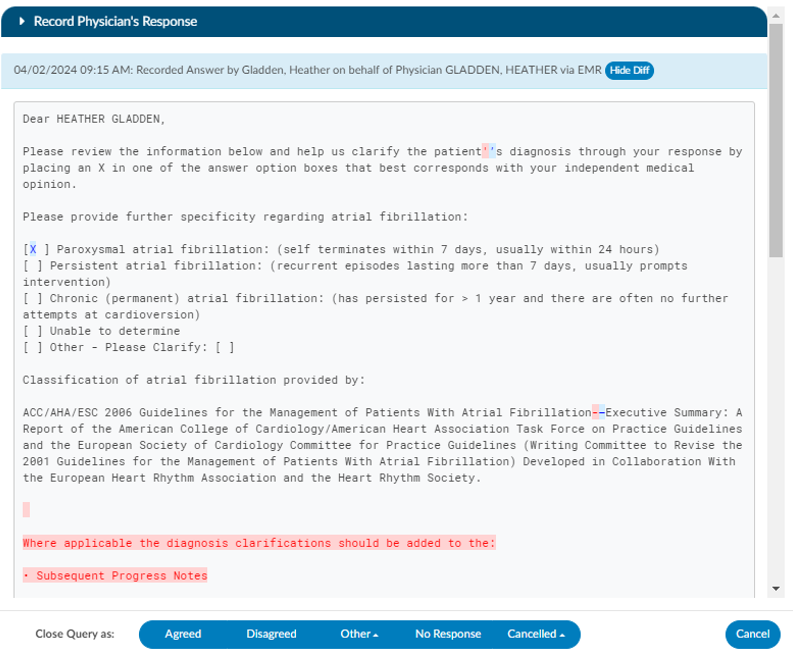
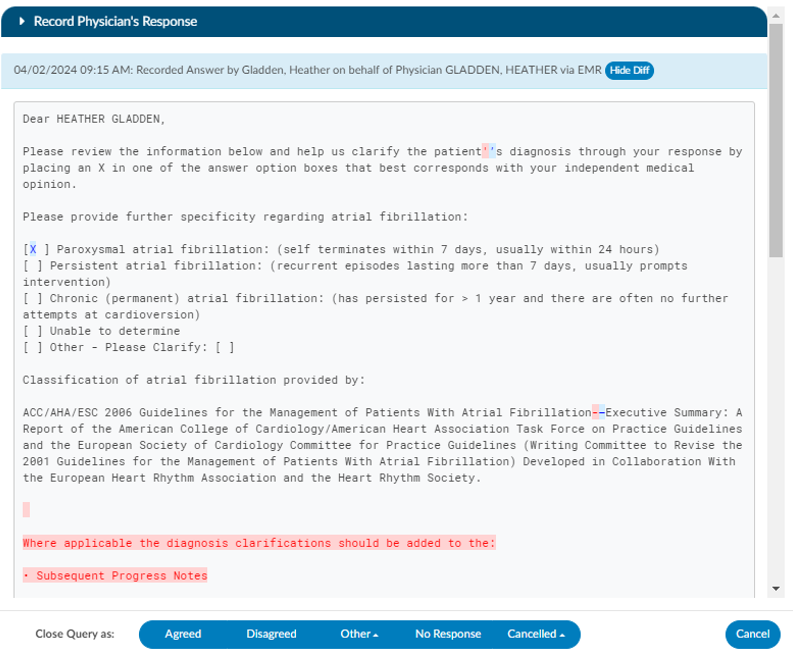
Each query is marked with a red envelope icon. Clicking this icon allows you to open the query and review its contents. Within the query review window, you may adjust the pre-DRG and post-DRG to reflect impact and then proceed to compliance evaluation.
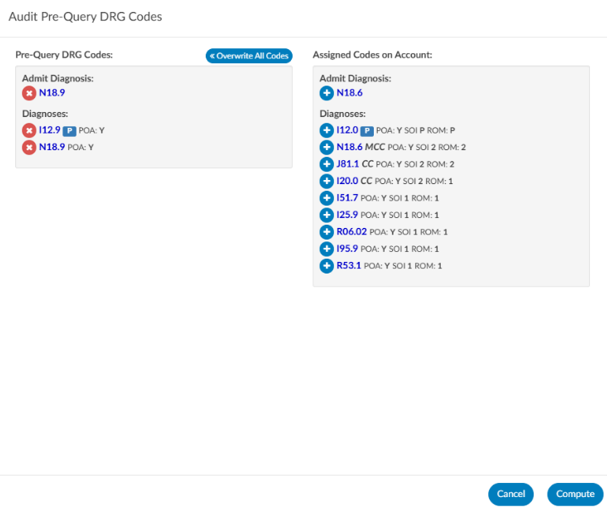
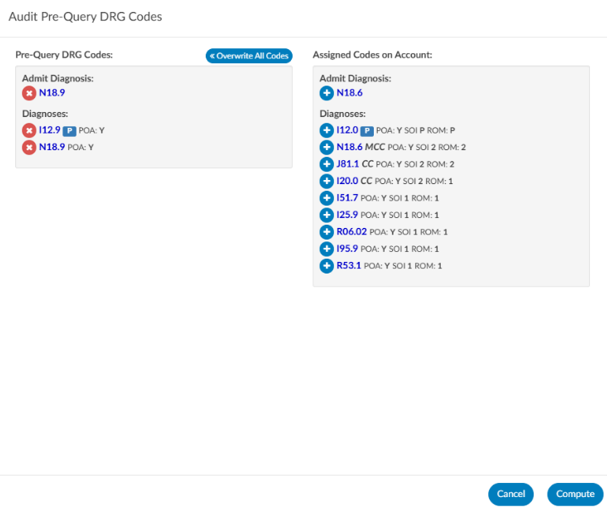
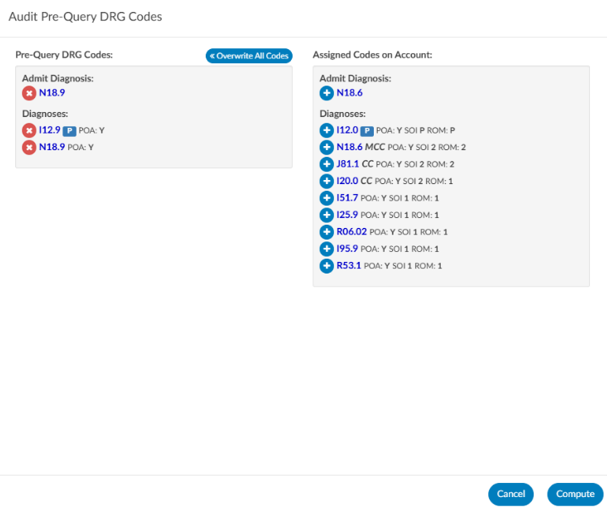
Query Pre/Post DRG
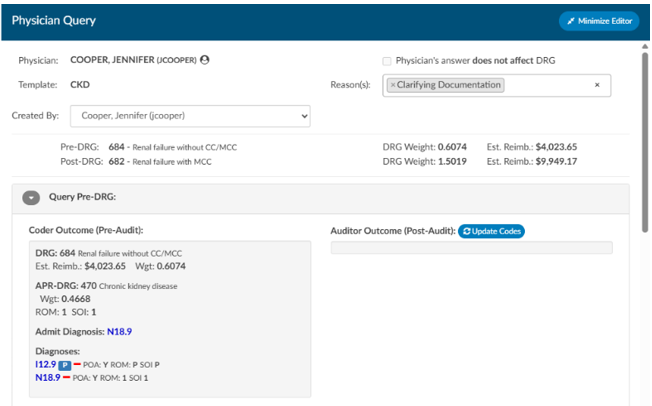
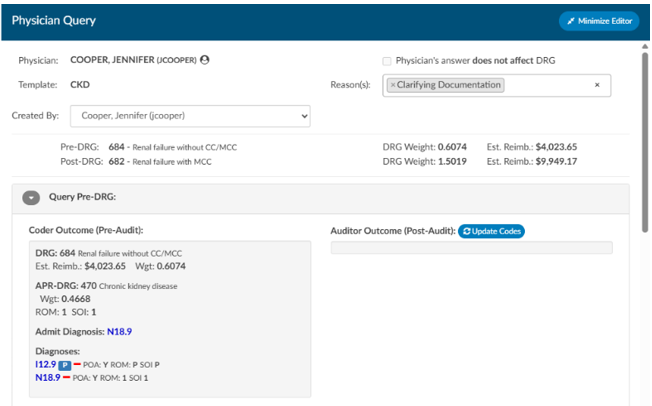
If either of the pre-DRG and/or post-DRG you can click to open either section. If you click on update codes. The editor presents two panels:
- Left side: Displays the codes used to calculate the current baseline DRG.
- Right side: Displays the system’s assigned code tree, showing all available codes. Move any codes from the right to the left if you want the audited Baseline to use these codes.
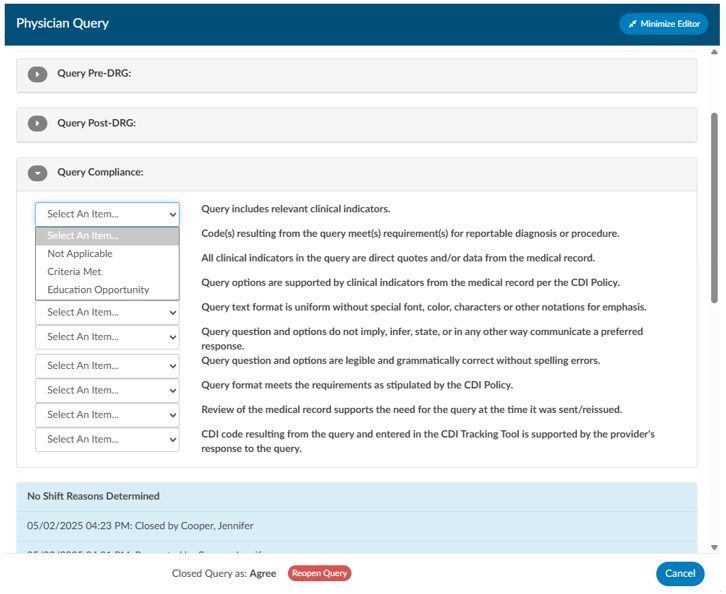
Query Compliance Questions
For each query, the system provides ten compliance questions. These are customizable through the mapping table but generally focus on ensuring that the query was appropriate, compliant, and educational.
Response options include:
- Not Applicable – The question does not apply to this query.
- Criteria Met – The query meets compliance standards.
- Training Opportunity – The query does not meet expectations and is counted as a negative finding.
Each query therefore has up to ten possible compliance opportunities. The number of “Training Opportunity” responses provides a measure of compliance performance. If an auditor identifies that a CDI missed sending a query that should have been issued, the auditor can document this as a Missed Query Opportunity. This requires opening the physician query section as you would normally and recording the oversight within the audit.
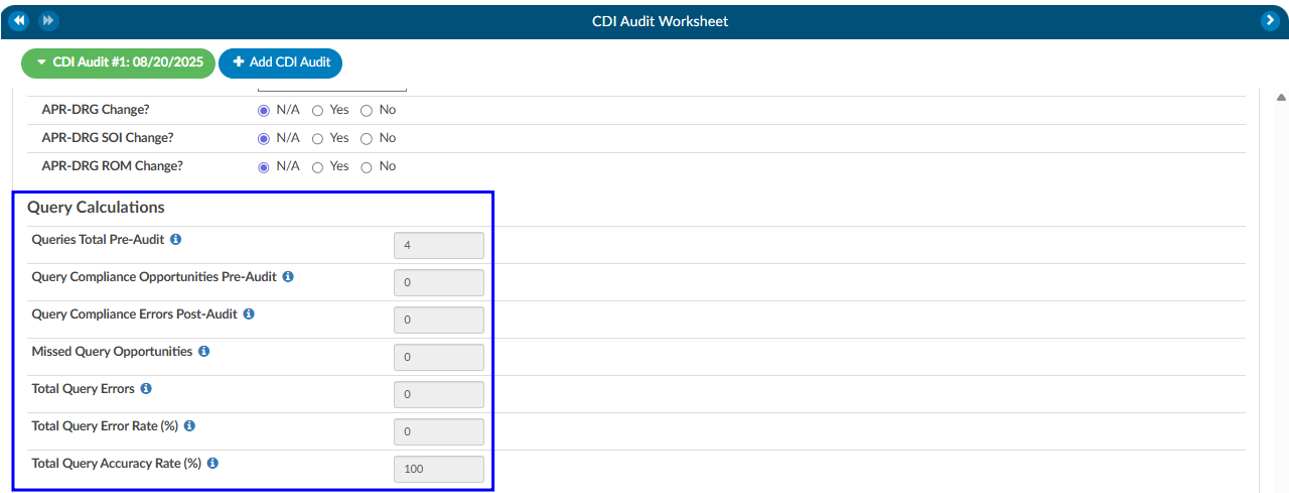
CDI Audit Statistics
Baseline/Working DRG Changes
If there are changes to the Baseline or the Working DRG this section will automatically move the radio buttons automatically to line up with the differences between the CDI Outcome compared to the Auditor Outcome.
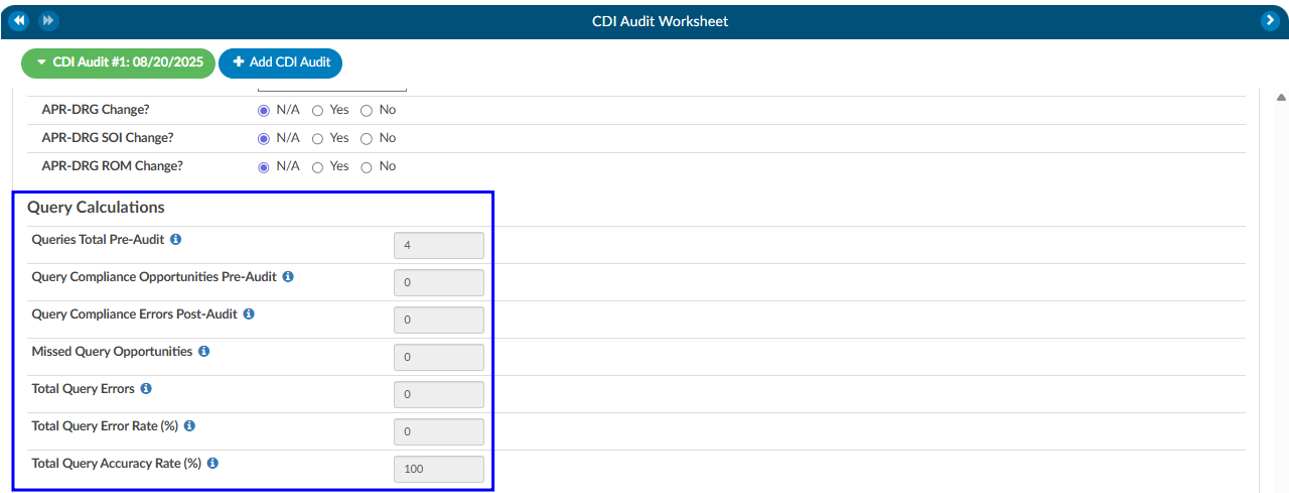
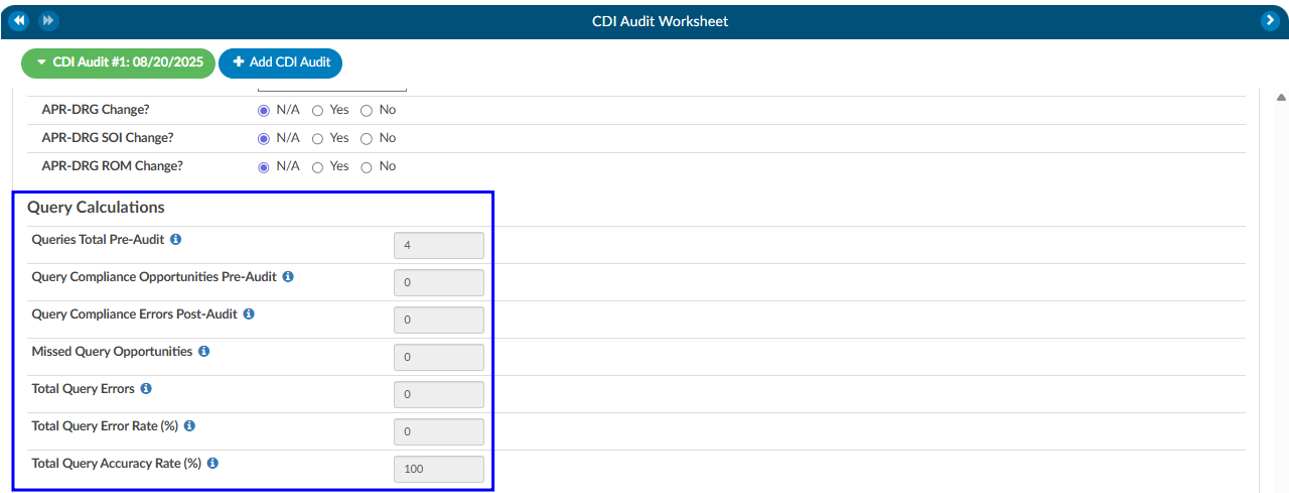
Query Calculations
The below calculations are the outcome of each query that was audited.
| Fields | Description |
|---|
| Queries Total Pre-Audit | This is the total queries pre-audit that was created by the CDI being audited that were not canceled. |
| Query Compliance Opportunities Pre-Audit | Query Compliance Opportunities that are labelled as criteria-met or educational-opportunity. |
| Query Compliance Errors Post-Audit | Query Compliance Opportunities that are labelled as educational-opportunity. |
| Missed Query Opportunities | Queries created by the CDI Auditor after this audit was started |
| Total Query Errors | Total Query Errors = Query Compliance Errors Post Audit - Missed Query Opportunities |
| Total Query Error Rate (%) | Total Query Error Rate (%) = (Query Compliance Errors Post-Audit + Missed Query Opportunities)/(Query Compliance Opportunities Pre-Audit + Missed Query Opportunities) |
| Total Query Accuracy Rate (%) | Total Query Accuracy Rate (%) = 100 - Total Query Error Rate (%) |
Training Recommendations
At the conclusion of the audit, the Auditor can list any recommended training topics. If no recommendations are necessary, “None” should be indicated. These topics can be modified using the mapping table. Additionally, the Auditor has space to provide any additional details as needed.
Best Practices
To maximize the effectiveness of CDI audits, auditors should follow several best practices. Always verify that you are auditing the correct CDI of record before starting, as this ensures you are reviewing the intended queries and DRGs. Use audit subtypes to capture specific learning opportunities, such as audits performed for new CDI staff or targeted reviews of certain DRG assignments. Ensure compliance questions are kept current, reflecting not only internal policies but also industry guidelines and payer expectations. Finally, conduct audits consistently and document findings clearly. Overtime, this creates a feedback loop that improves documentation quality, strengthens DRG accuracy, and reinforces compliance across the CDI program.
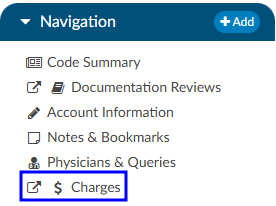
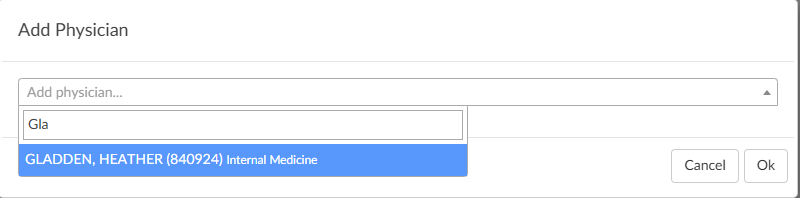
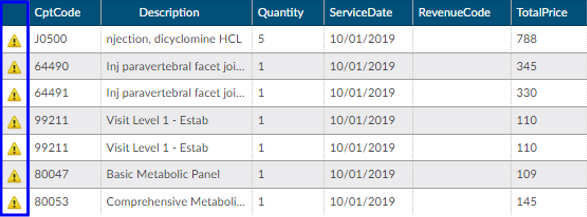
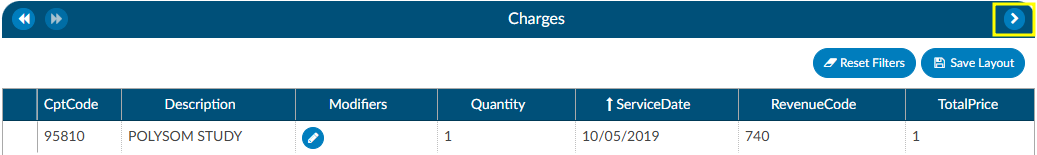
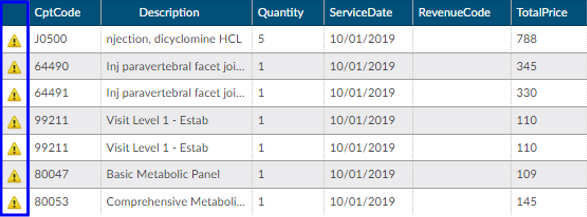
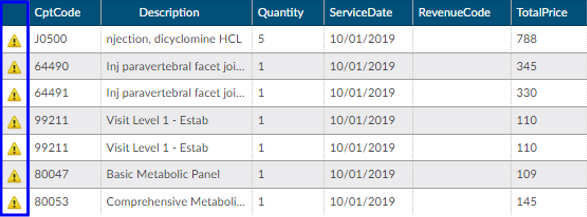
Charges or Transactions
If an interface for account charges or transactions is set up during configuration, the Charges viewer shows a listing of charges on the account.
There are activity buttons to “Save Layout” or expand the Charges viewer. Users can expand the width of the Charges viewer to view more available columns by clicking on the arrow in the top right corner of the viewer. This viewer also provides information on CPT Codes, Descriptions, Modifiers, Quantity, Service Date, Revenue Code, and Total Price.
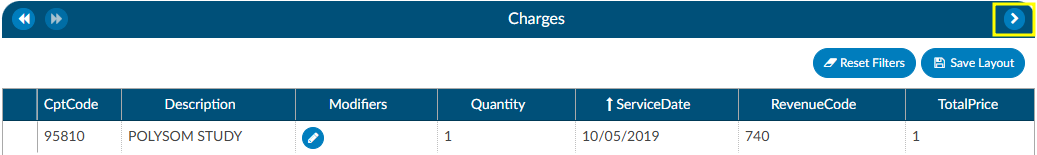
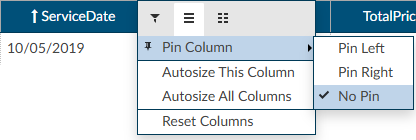
Column Settings
Each column within the Charges grid has menu options to Pin Column, Autosize, and Reset Columns. Click on the Menu icon to view the drop-down listing. After making column setting selections, click on the button to retain column settings for future coding sessions.
| Column Setting | Definition |
|---|
| Pin Column | Allows users to select the column and then pin it to the RIGHT or LEFT side of the assigned accounts grid. This function works similarly to freezing columns in Excel. |
| Autosize This Column | Select this option to change the column width to automatically size the width of the column for contents of the cells in this column. |
| Autosize All Columns | To quickly autosize all columns in the assigned accounts grid, click the Autosize All Columns button. |
| Reset Columns | Click on this option to Reset Columns to their default column width. |
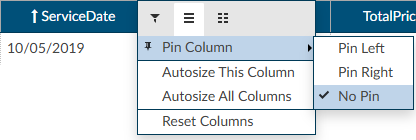
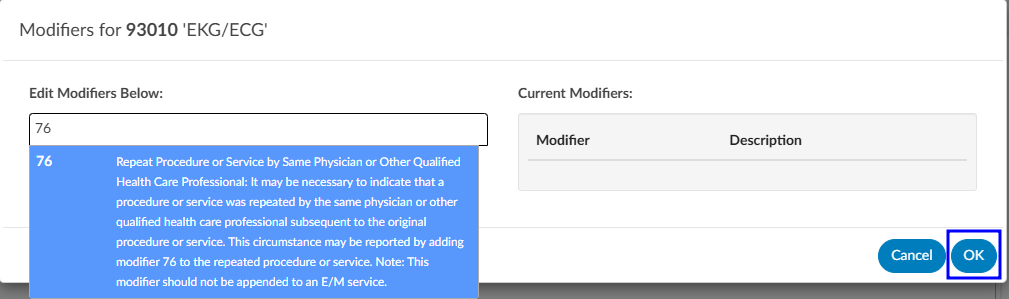
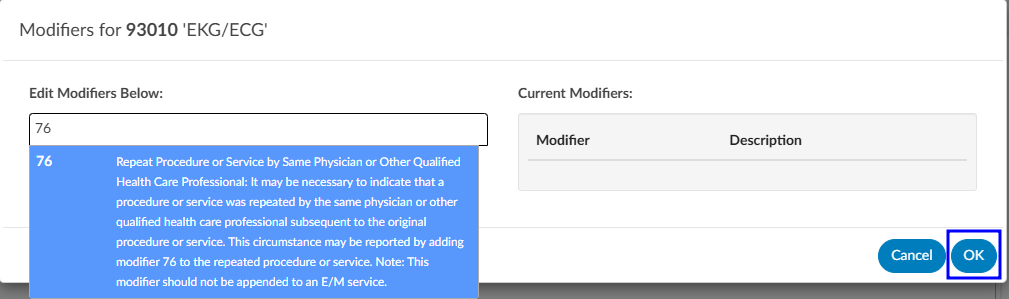
Adding Modifiers to Charges
Click on the BLUE PENCIL
button to open the Modifiers window. Start entering the digits for the modifier to bring up the drop-down listing of available modifiers and their descriptions to select the appropriate modifier. After the modifier is in the window, click on the OK button to save the selected modifier. Continue this process to add all applicable modifiers to charges in the Charges viewer. The user can add up to four (4) modifiers unless they are using the Solventum CRS encoder, then they will be able to add up to five (5) modifiers.
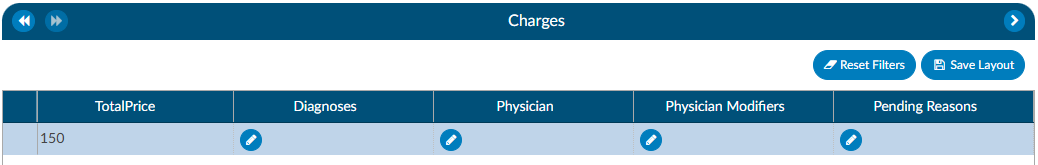
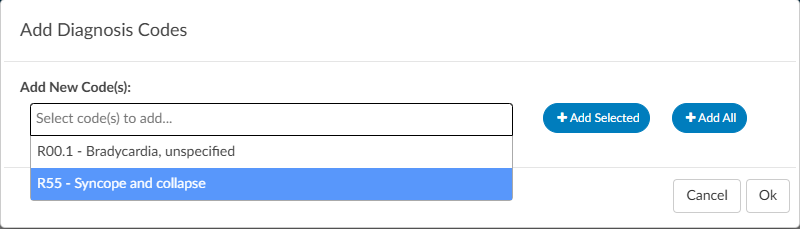
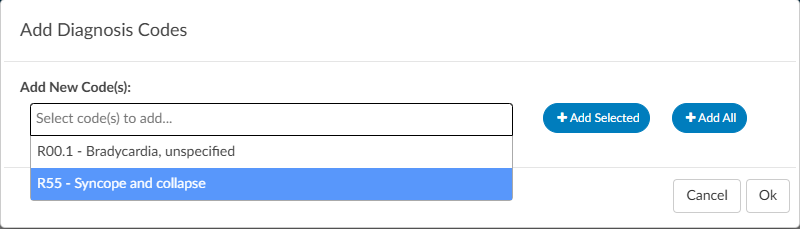
Editing Hard Charge Details (Physician Coder)
A user with the role of a Physician Coder can now add assigned diagnosis codes along with physicians and CPT Modifier codes to hard charges listed in the Charges viewer. When a Physician Coder opens the Charges viewer, new columns with edit buttons will be seen.
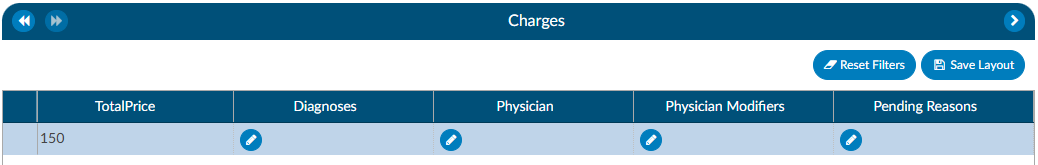
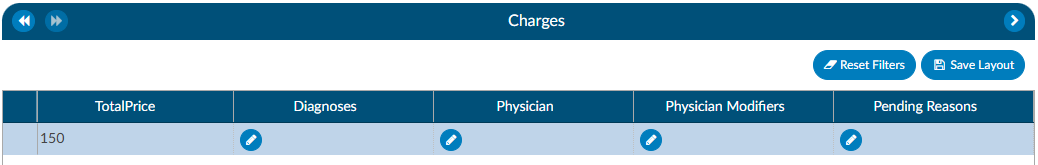
Clicking on the BLUE PENCIL
button in the Diagnosis column will open a code field, which when dropped down, will list all assigned diagnosis codes on the account. The Physician Coder can then select which diagnosis code(s) to attach to the hard charge. The top most diagnosis code of a charge is designated the “principal” diagnosis. If you add or remove codes, whatever code is listed first is the principal – the principal code on a charge can be different than the principal code on the account. If a user moves the codes around, the top code will always become the primary code.
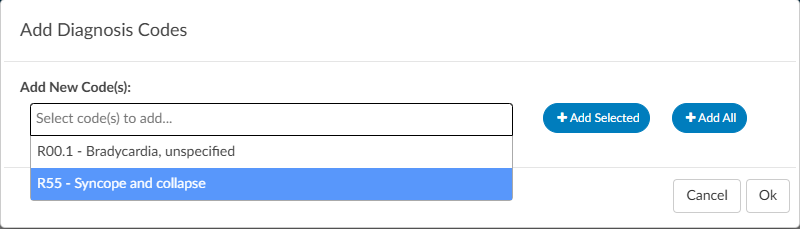
Clicking on the BLUE PENCIL
button in the Physician column will open a physician field to allow the selection of a physician. This is the same for the Physician Modifiers column which will open a modifier window allowing modifiers to be selected. When launching the encoder, the physician coder’s modifiers will be sent instead of the final modifiers in the Charges viewer.
Clicking on the BLUE PENCIL
button in the Quantity column will open a field to allow the end user to enter a new value for the quantity of the charge. The dialog will perform validation so that invalid quantities are not recorded such as letters, blanks, and/or a zero quantity. Negative quantities are permitted. Decimal quantities are permitted.
Note
The organization must have physician coding enabled to use this feature, if you do not have physician coding please contact your account representative for more information.
Assigning a Pending Reason per Charge (Single Path & Physician Coder)
Users that have a Physician Coder or Single Path Coder role will have the ability to place a pending reason per charge on the physician charges.
- If a charge is removed, then the pending reason would be removed.
- If a charge is updated, then the pending reason would not change.
Caution Column (TruCode)
A Caution Column is avaialble for sites that use the TruCode Encoder to the Charges and Transactions viewers. This column will indicate a flag if TruCode reports an edit on a charge on an outpatient account.
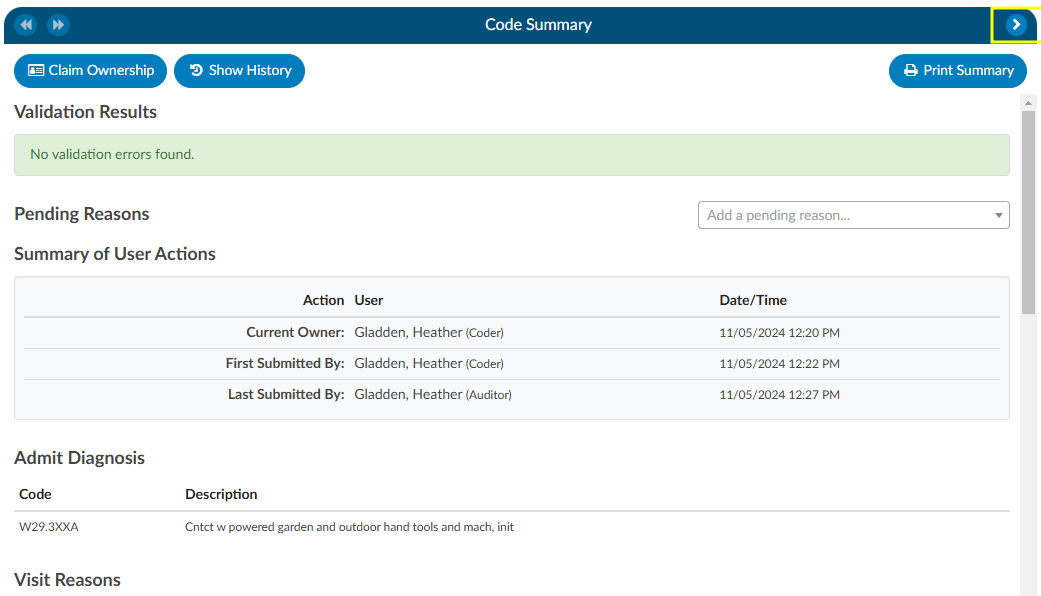
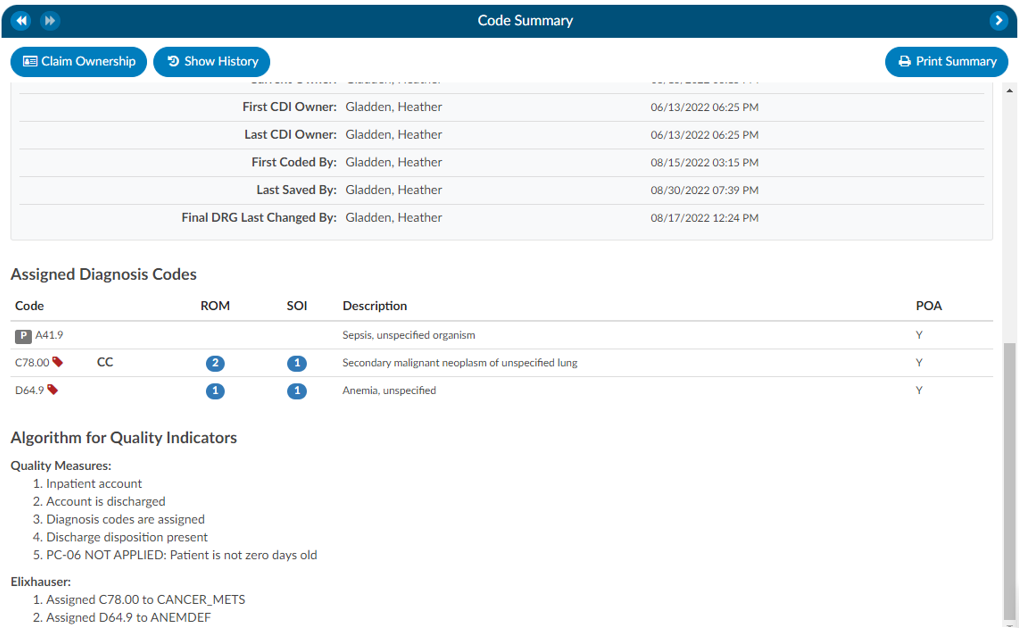
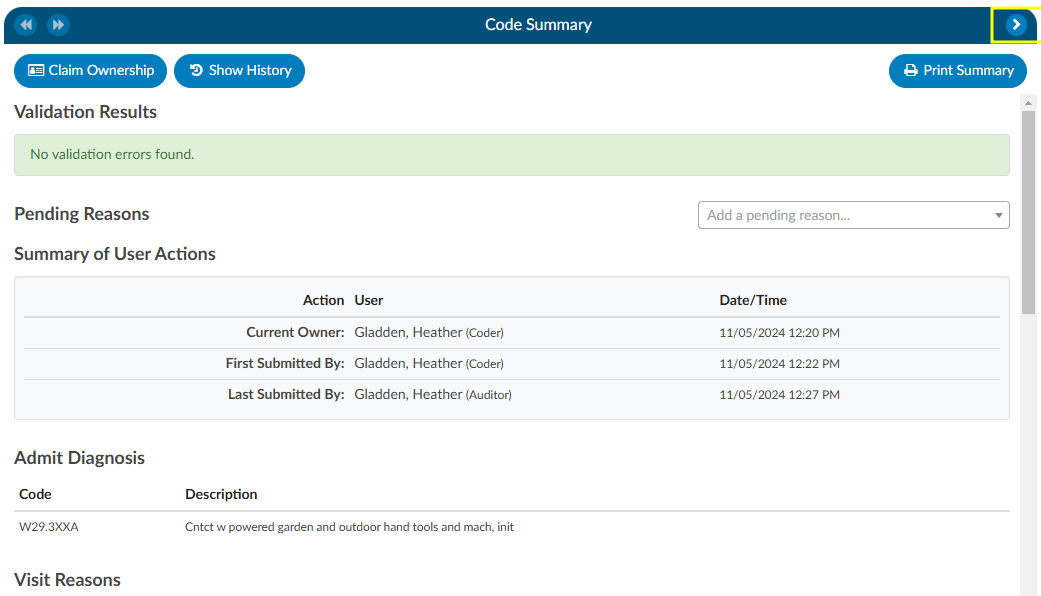
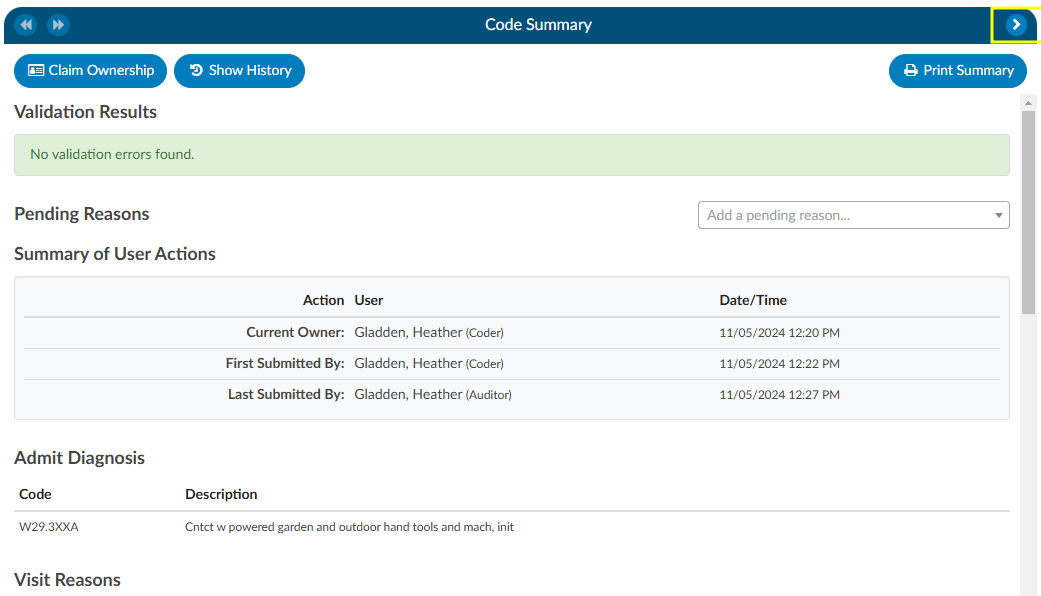
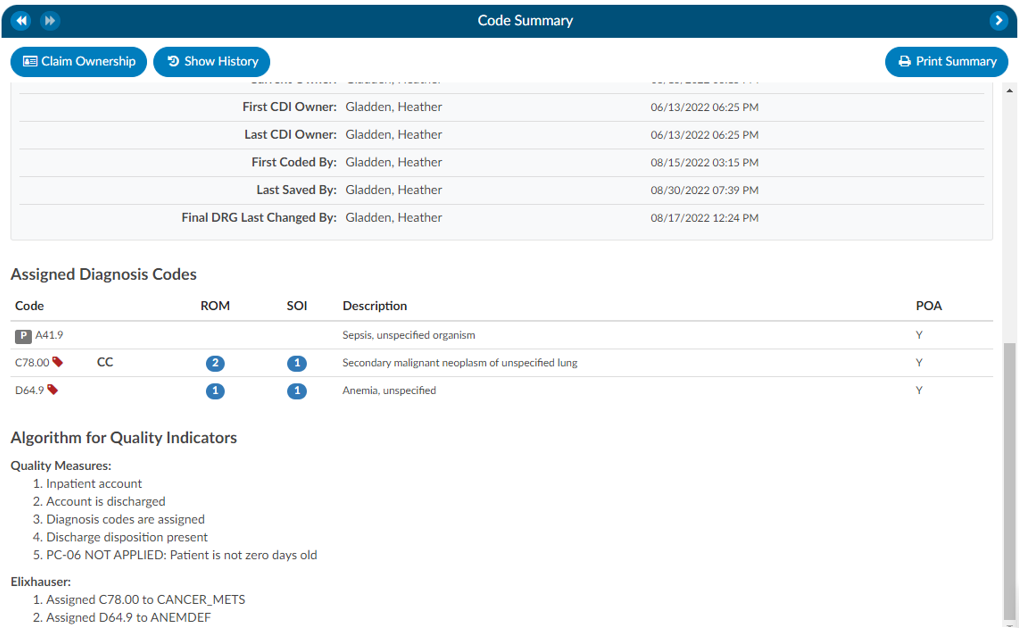
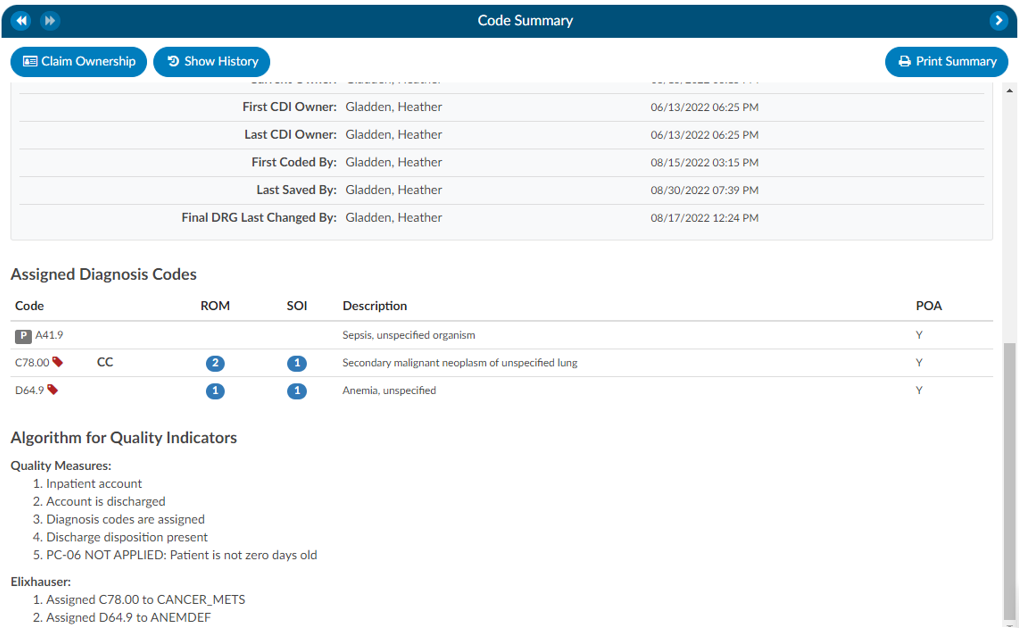
Code Summary
The Code Summary is the last viewer to be reviewed prior to chart submission. This screen shows a summary of activity on the account and provides activity buttons to Claim Ownership, Show History, and Print Summary (if a printer is configured). This viewer also provides information on Current Owner, First Coder, Last Saver, and Last Submitter. Users can expand the width of the Code Summary viewer by clicking on the arrow in the top right of the viewer.
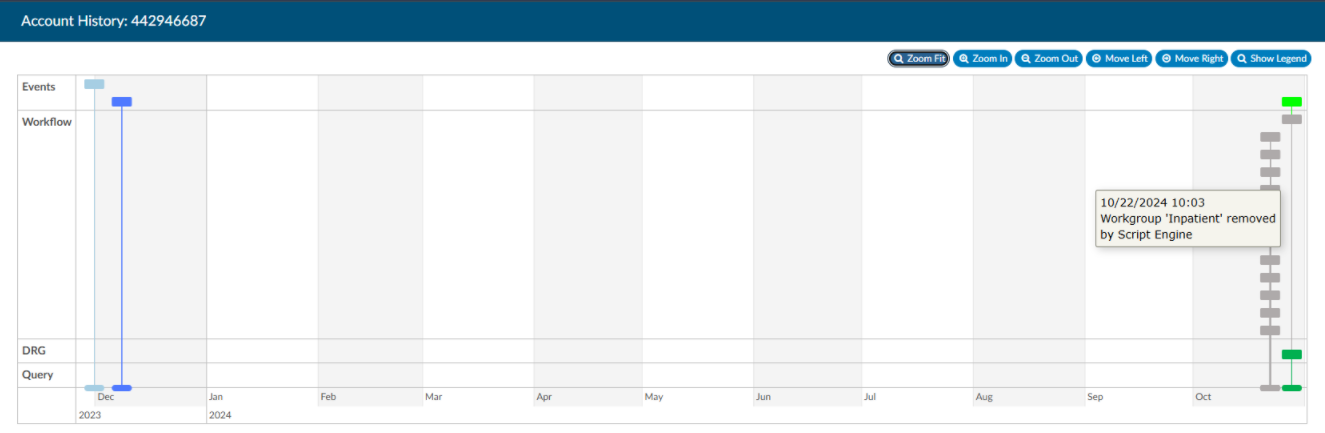
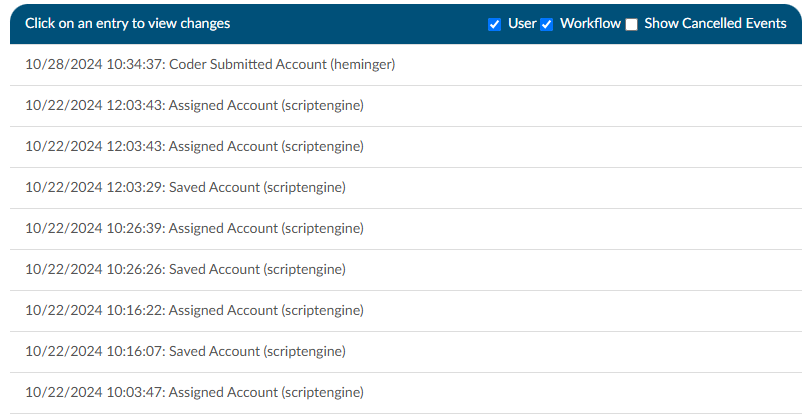
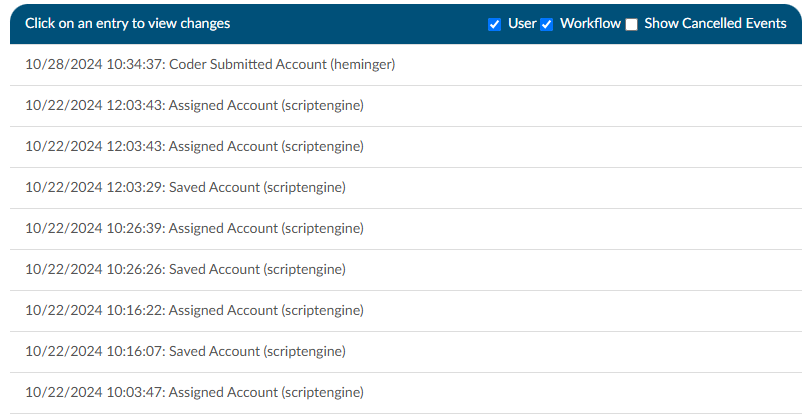
Show History
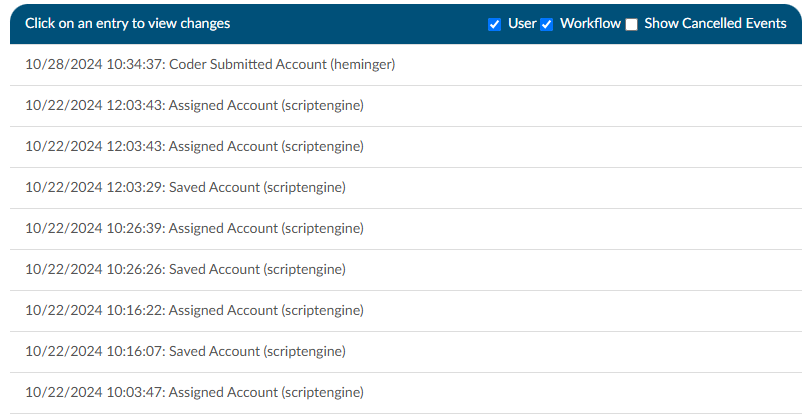
The Show History button provides a timeline view of activity on the account along with an audit trail of account activity from point of admission to the current date. It includes a visual timeline and below the timeline there will be an audit trail of account activity.
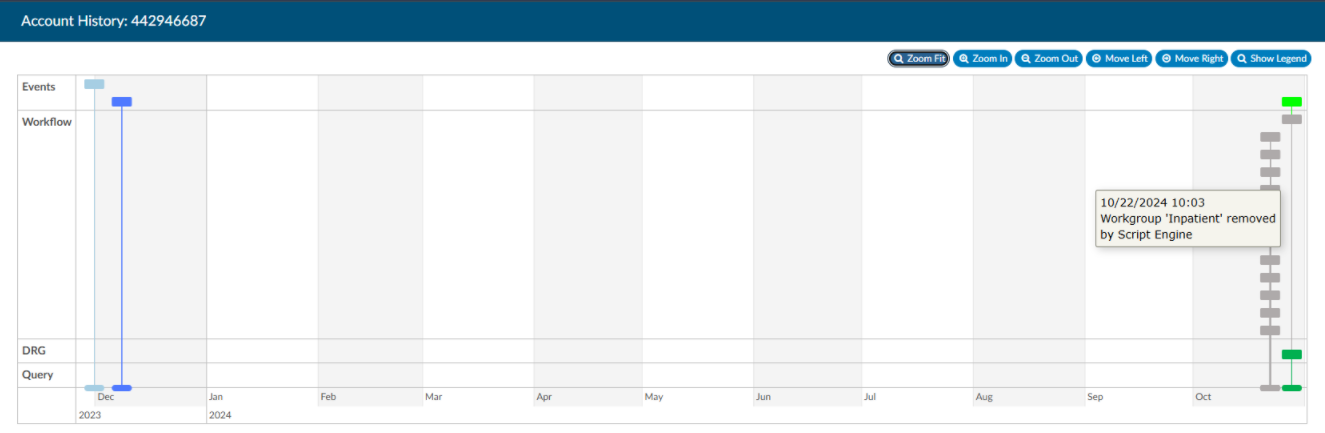
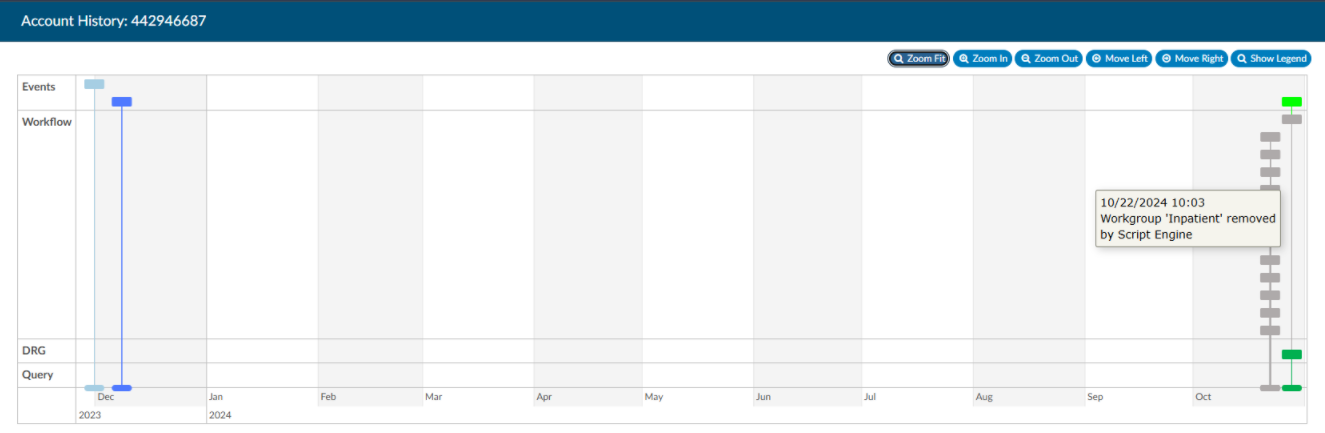
Upon opening Show History, users will see the entire history from a birds-eye view. The user has the option of using the Zoom In and Zoom Out buttons to expand or collapse the timeline. The Zoom Fit will bring the visual timeline back to its original collapsed grid. Hover over any of the event boxes and the contents will be displayed.
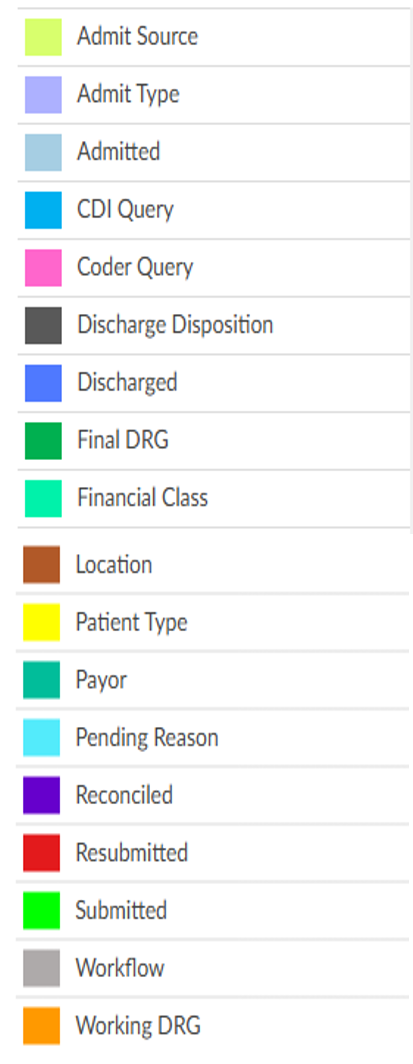
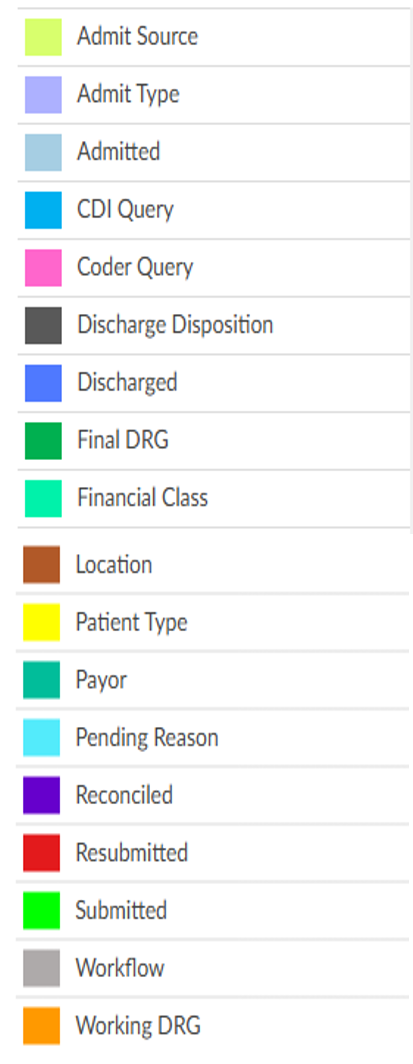
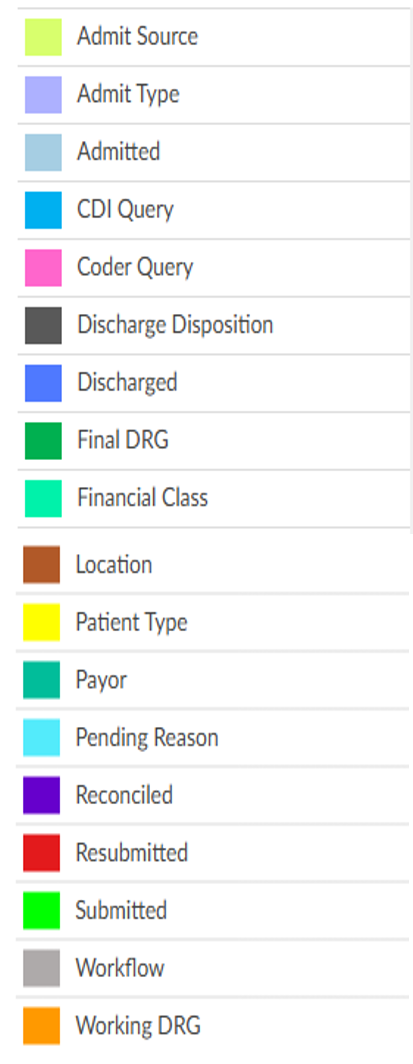
The legend can be found by clicking Show Legend to let the user know what the colors represent without having to hover over them. When clicked, it will open the Legend and the button name will change to “Hide Legend”. Click again to close.
Click on an entry by date to view the changes that were made to the account on the date and time indicated.
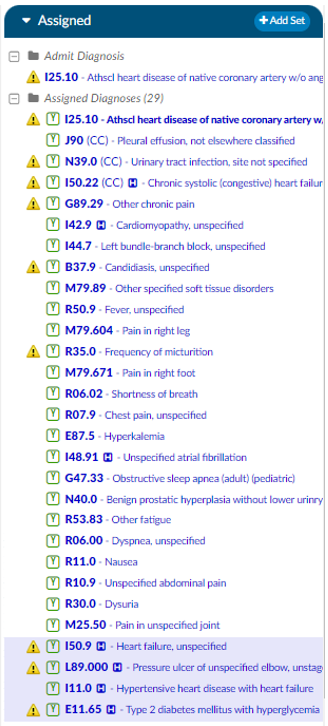
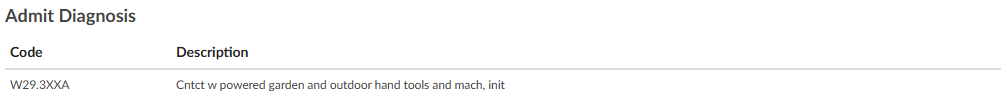
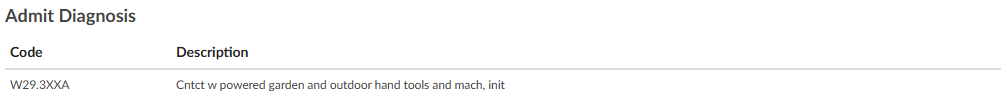
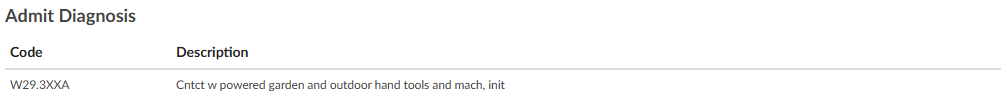
Admit Diagnosis
The Admit Diagnosis code and description are displayed below any Validation Results and/or Pending Reasons.
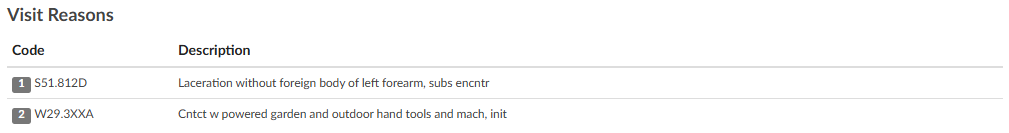
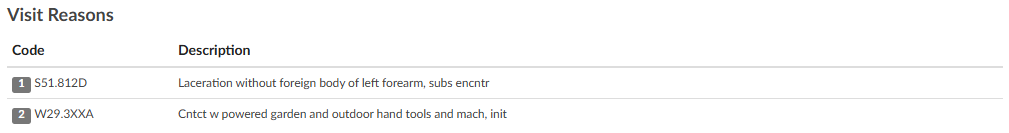
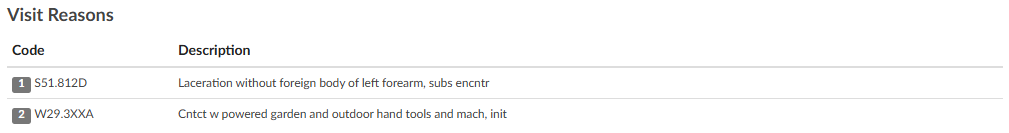
Visit Reasons
Listed beneath Admit Diagnosis are the Visit Reason codes in code sequence order. The list includes the Visit Reason code and description.
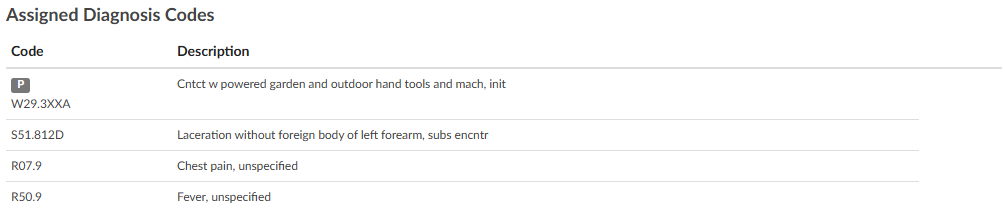
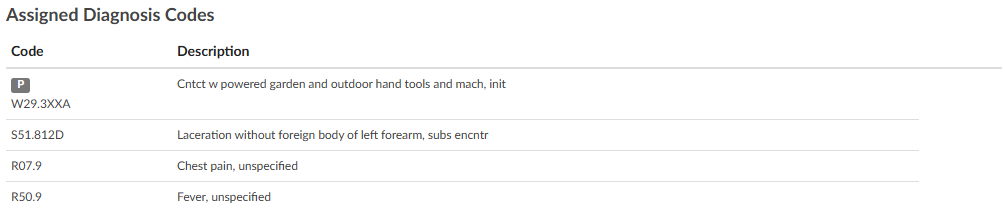
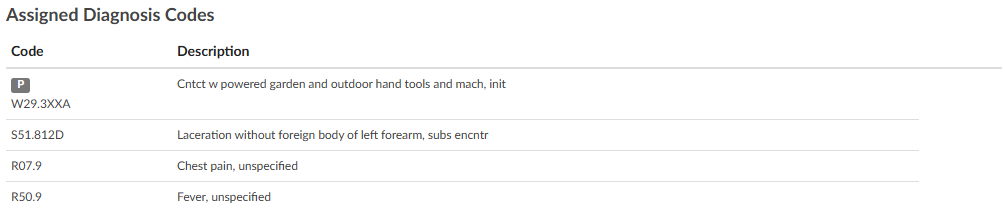
Assigned Diagnosis Codes
The Assigned Diagnosis Codes are listed in code sequence order below Visit Reasons. The listing includes the diagnosis code, description, and POA assignment (Y/N).
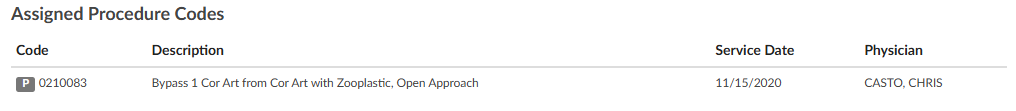
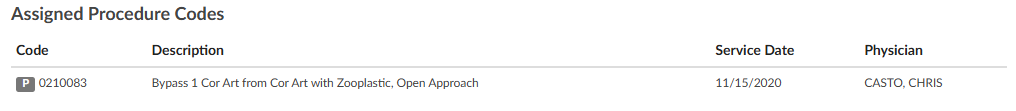
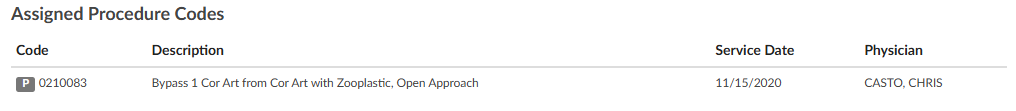
Assigned Procedure Codes
Listed beneath Assigned Diagnosis Codes are the Assigned Procedure Codes in code sequence order. The list includes the procedure code, description, Service Date, and Physician.
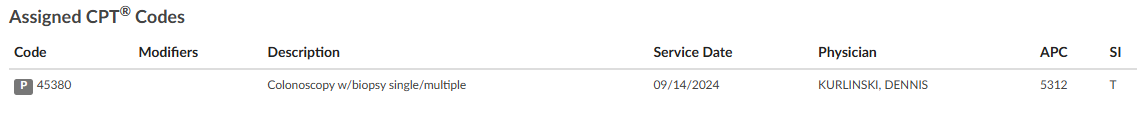
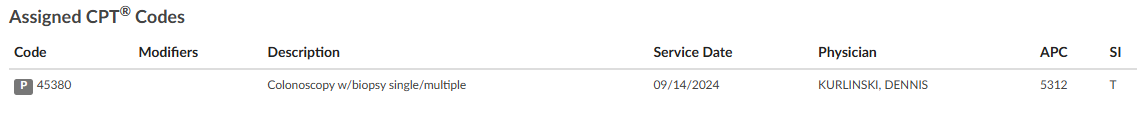
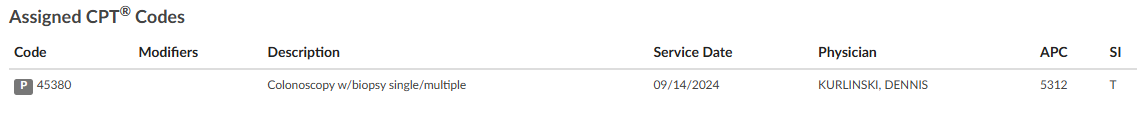
Assigned CPT Codes
Listed beneath Assigned Procedure Codes are the Assigned CPT Codes in code sequence order. The list includes the CPT code, Modifiers, Code Description, Service Date, Physician, APC and Servier Indicator.
Print Summary
If a printer is configured for the computer, click on this button to print a copy of the abstract for this account.
Claim Ownership
Use the Claim Ownership feature based on the organization’s requirements and procedures. Consult your manager for more information on claiming ownership of a chart.
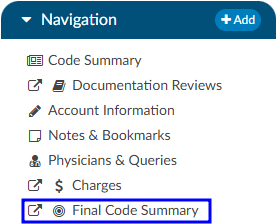
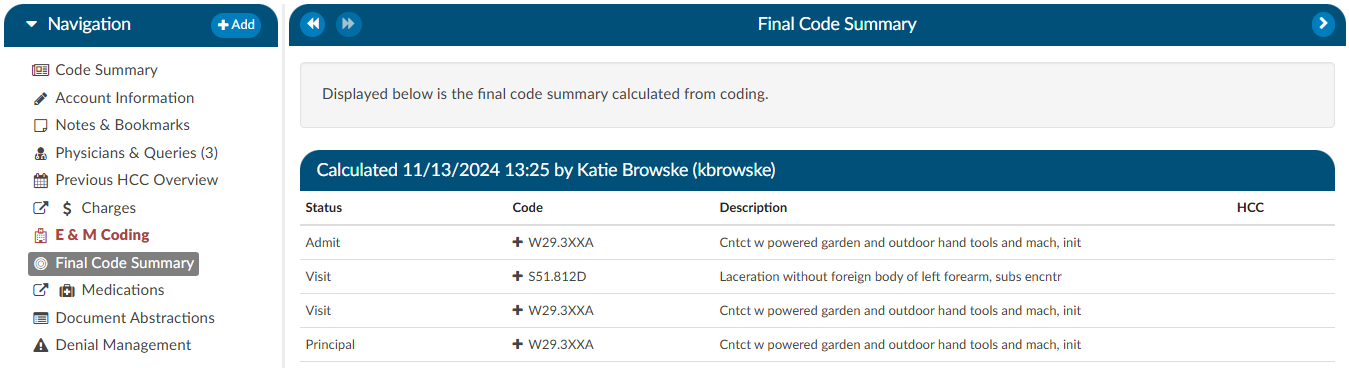
Final Code Summary
The Final Code Summary will only be available once the facility Coder clicks the Submit button. This provides transparency between CDI and physician coding teams (if also using Fusion CAC) as to what was coded. When a submitted chart is open again, users will see a new viewer under the navigation menu called the Final Code Summary. This will display what the coders coded along with code status details and sequencing. This data is viewable only for the role of ‘CDI’.
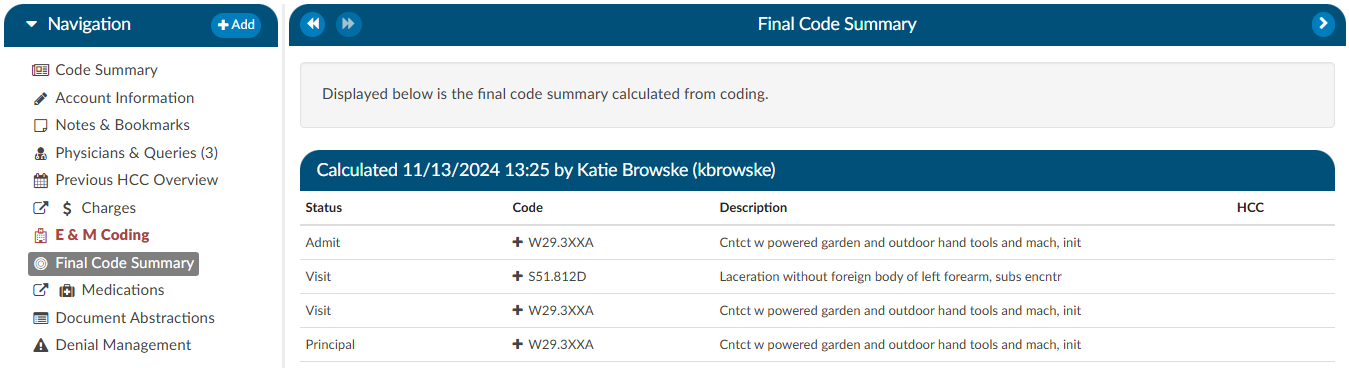
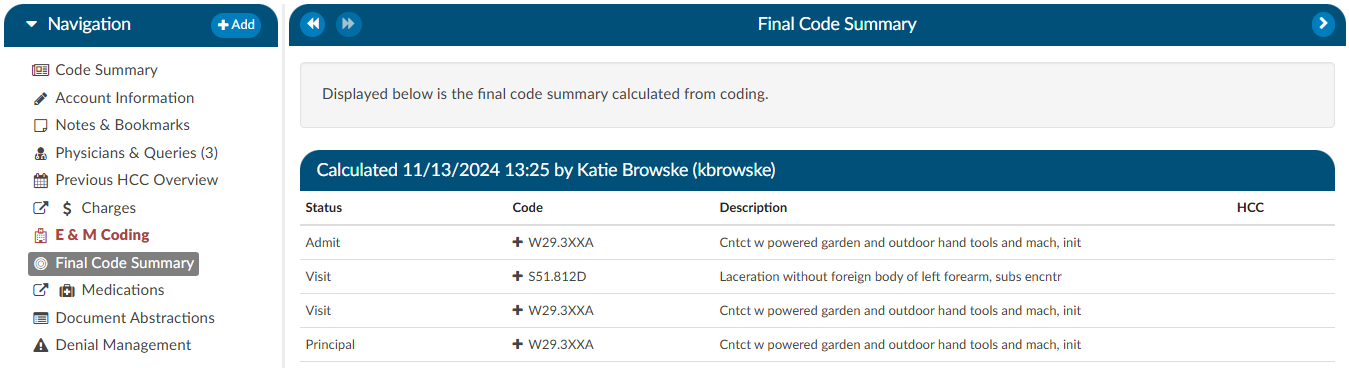
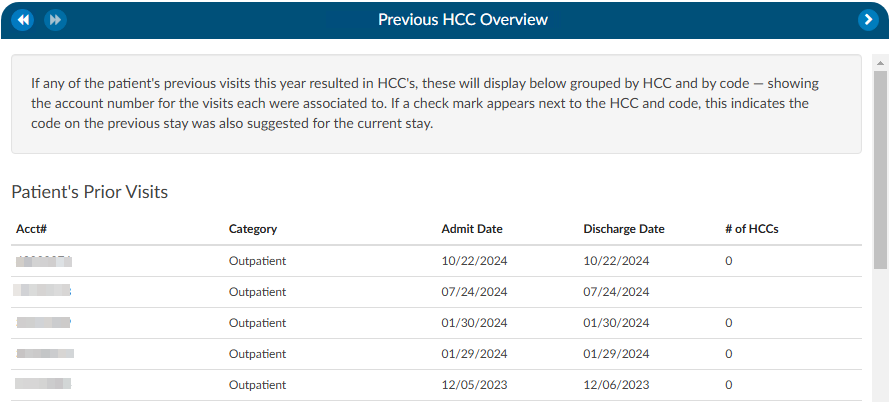
Clicking on the header will expand the selection to display the codes that were coded and DRG/APC, if applicable. Any codes with a plus (+) sign indicates the code has not been added to the account. The plus (+) sign does not indicate that the code needs to be added. It is for the user to quickly add the code if they determine it is needed using coding judgment and supporting documentation. If applicable, the code’s HCC designation will show the HCC number and its version.
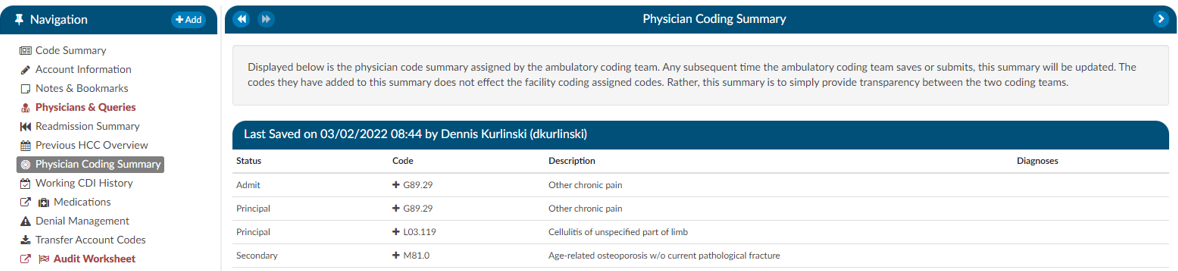
Physician Coding Summary
The Physician Code Summary will display if the Physician Coders are also coding within Fusion CAC, and they submit the chart. This provides transparency between the facility and physician coding teams as to what was coded.
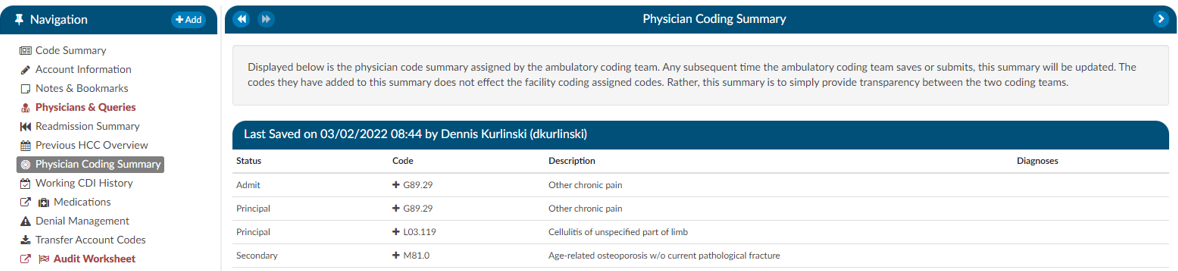
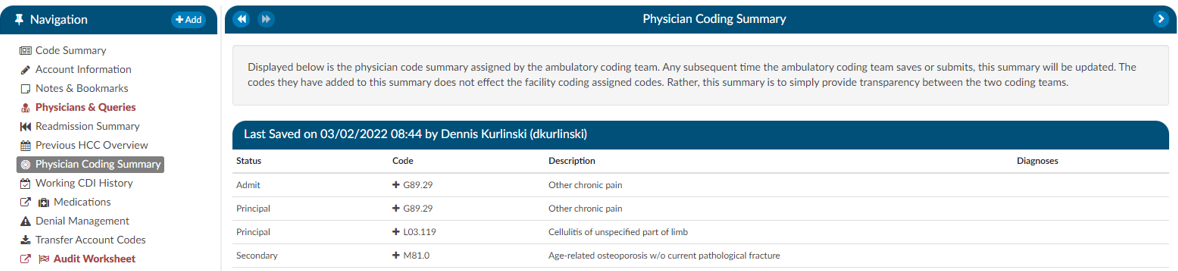
Clicking on the header will expand the selection to display the codes that were coded. Any codes with a plus (+) sign indicates the code has not been added to the account. The plus (+) sign does not indicate that the code needs to be added. It is for the user to quickly add the code if they determine it is needed using coding judgment and supporting documentation.
Subsections of Code Summary
Pending Reasons
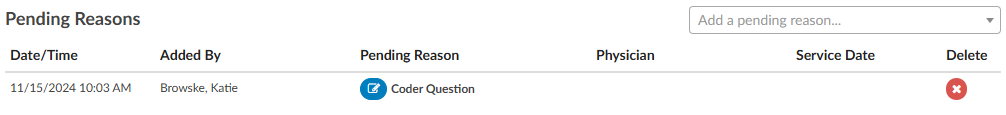
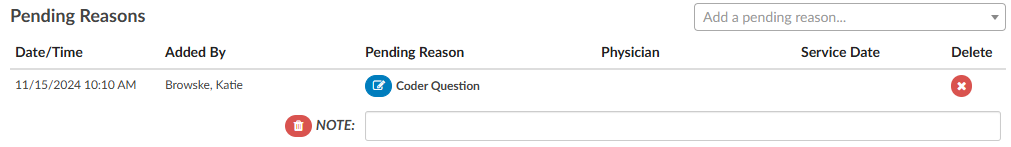
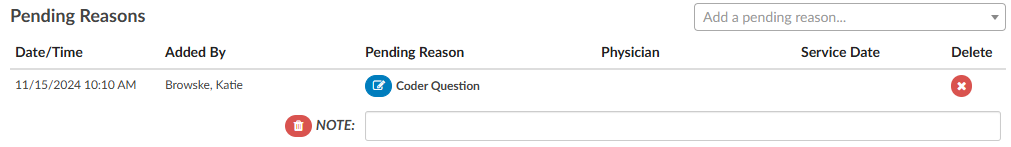
Pending Reasons
A list of Pending Reasons assigned to the account can be found within the Code Summary viewer below Validation Results.
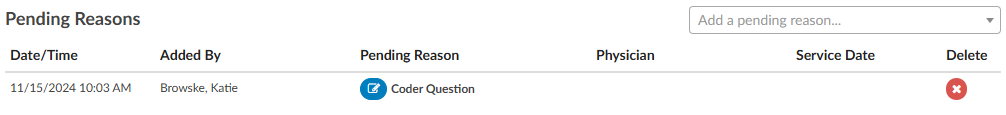
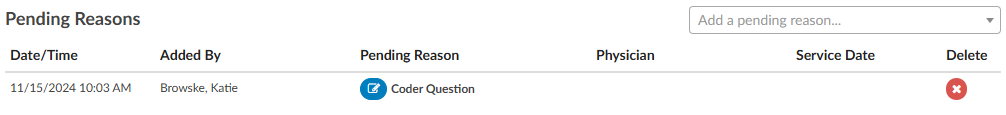
Pending reasons are used when a chart cannot be completed or routed to another Workgroup. The number of pending reasons selected is unlimited. Pending reasons will be different for each facility based on system configuration specifications. Please contact your manager for definition and use of available pending reasons.
Pending Reasons can be added to the account by clicking on the drop-down menu and selecting the applicable Pending Reason. If the organization has selected to allow a physician to be tied to a pending reason, the user will be prompted to assign a physician to the pending reason, and will see an additional physician field in the list of pending reasons.
If physicians have been turned on for pending reasons, not all pending reasons may be tied to a physician. This option is set within the mapping configuration.
If a pending reason is added to an account, the Submit button will be grayed out and unavailable. Click on the Save button to save all changes and exit the chart. Charts with pending reasons will stay within the existing Workgroup until the Pending Reason is removed. Pending Reasons can also be deleted/removed from accounts by clicking on the “X” next to the Pending Reason to be removed.
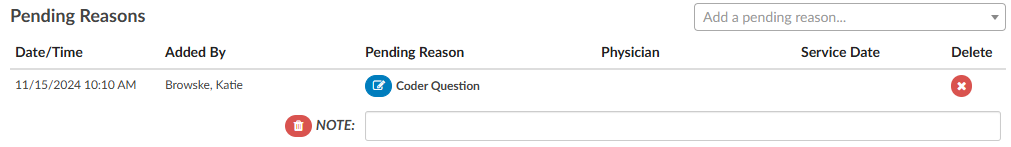
Pending Reason Notes
On any account, an edit button will appear to the left of the pending reason. Clicking that button will drop down a note entry where the user can record a note. Pressing ENTER will record the note. Keep in mind that a note can be deleted by clicking a trash can symbol to its left. In Account Search, the “Pending Reasons” drill down will now include the “Note” field.
Quality Indicators
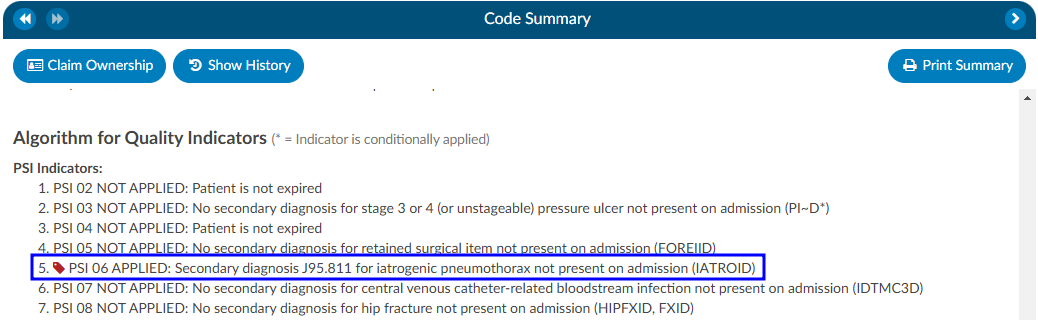
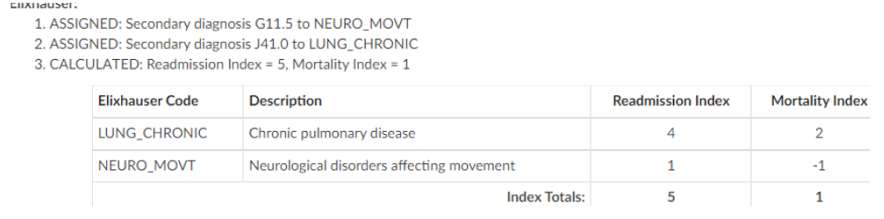
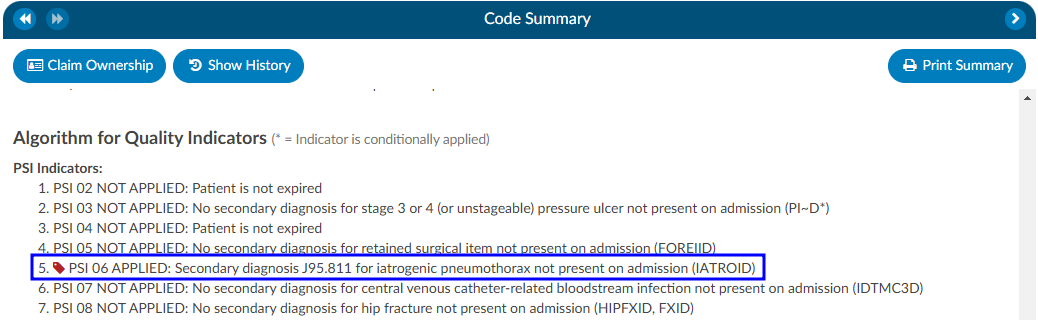
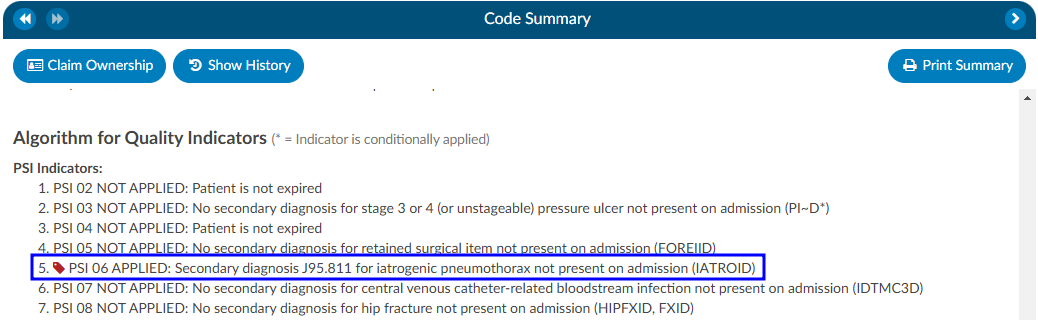
In the Code Summary Viewer at the bottom, you’ll find the Algorithm for Quality Indicators, which outlines the methodology used to identify Pediatric Quality Indicators (PDI), Patient Safety Indicators (PSI), Quality Measure PC-06, and Elixhauser Measures.
PSI Indicators
The PSI Module uses the PSI technical specification from Agency for Healthcare Research and Quality
U.S. Department of Health and Human Services from www.qualityindicators.ahrq.gov.
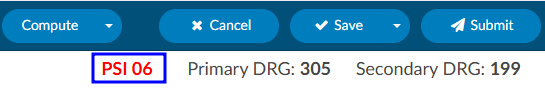
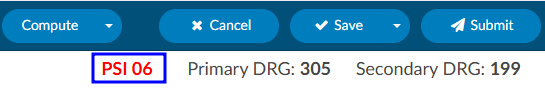
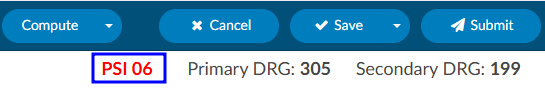
Fusion CAC leverages the codes from the assigned code tree, along with other relevant patient data, to determine whether specific quality measures are met. Fusion CAC provides an indicator on the banner bar when codes coupled with patient demographics meet a PSI guideline.
The PSI is reported in one of two fields CDI PSI Indicator or PSI Indicator. The indicator can be used for workflow and/or reporting. When a PSI is applied to an account it will display in the algorithm section of the Code Summary viewer. A red tag will display next to the applied PSI for visibility.
PDI Indicator
The PDI Module uses the PDI technical specification from Agency for Healthcare Research and Quality
U.S. Department of Health and Human Services www.qualityindicators.ahrq.gov.
The Pediatric Quality Indicators (PDIs) focus on potentially preventable complications and iatrogenic
events for pediatric patients treated in hospitals and on preventable hospitalizations among pediatric
patients, considering the special characteristics of the pediatric population.
This PDI indicator displays in the banner bar under the compute button. The PDI is reported in one of two fields CDI PDI Indicator or PDI Indicator if identified. The indicator can be used for workflow and/or reporting.
The algorithm for the PDI on if it applied or not is within the Code Summary viewer.
If a code that causes an exclusion for a PSI or PDI occurs in the top 25 codes (or custom limit set by the organization) the PSI/PDI will show in the banner, with an asterisk next to it, to indicate the PSI was conditionally applied. The algorithm at the bottom of the Code Summary viewer will show the reason why.
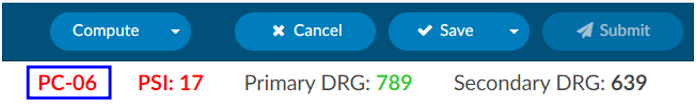
PC-06 Indicator
The Quality Measure Module supports the PC06 measure and uses the Joint Commission technical
specification https://manual.jointcommission.org/releases/TJC2018B/MIF0393.html.
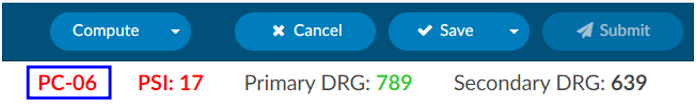
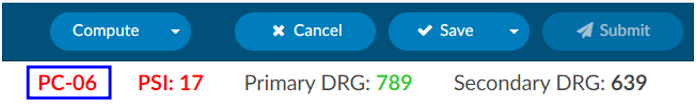
Fusion CAC uses the codes from the assigned code tree along with other patient data that meet each PC-06
guideline. Fusion CAC provides an indicator on the banner bar to a coder when codes coupled with
patient demographics meet a PC-06 guideline. The indicator can be used for workflow and/or reporting.
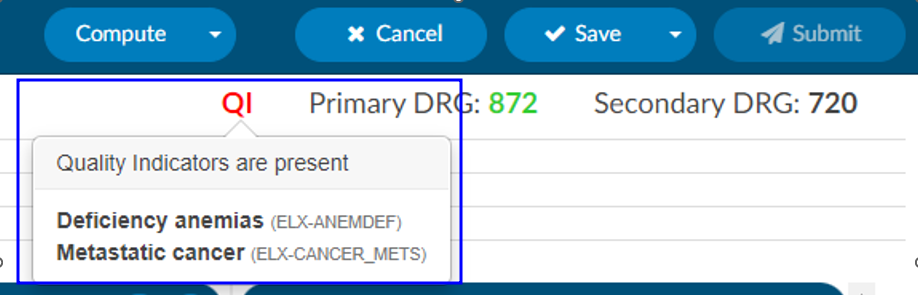
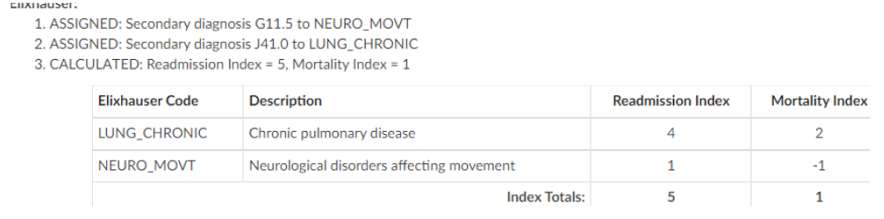
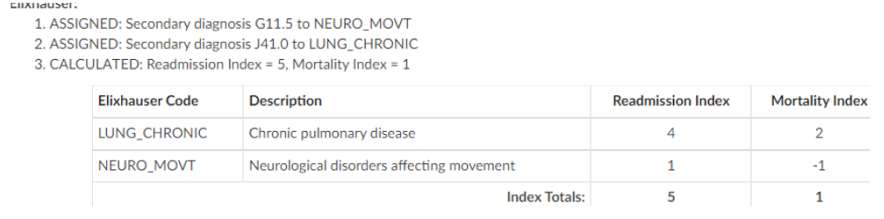
Elixhauser Comorbidity Measure Indicator
The Elixhauser Comorbidity Index is a method of categorizing comorbidities of patients based on the
International Classification of Diseases (ICD) diagnosis codes. The indicator can be used for workflow
and/or reporting.
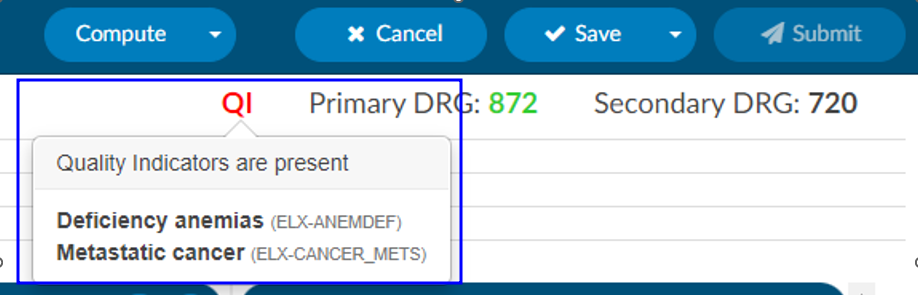
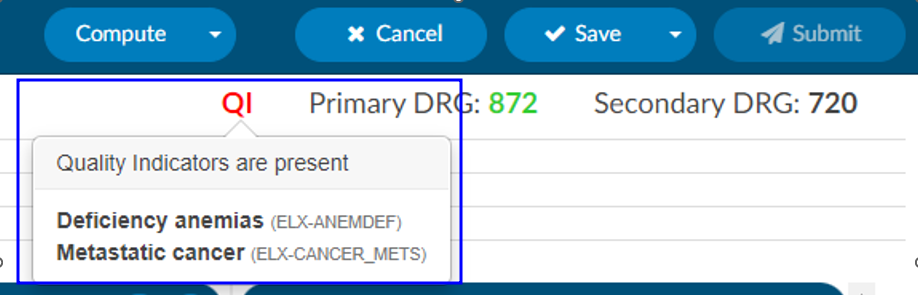
The algorithm to determine the Elixhauser measure can be found on the code summary at the bottom under the assigned codes. A table under the Elixhauser section of the Code Summary sheet will appear, showing weight totals for each item that triggers.
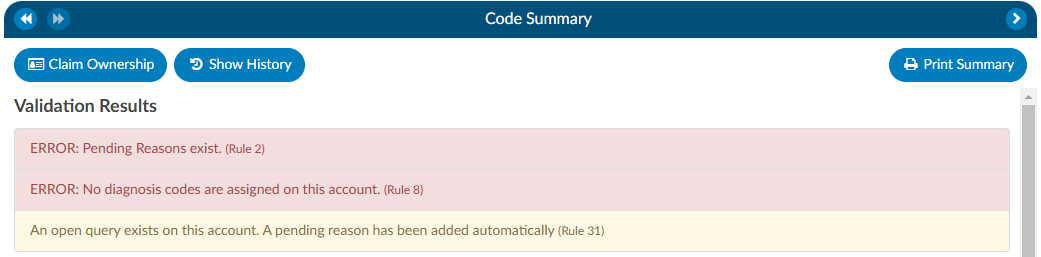
Validation Results
When the Code Summary link displays RED
, there are validation errors on the chart that must be resolved prior to submission.
Any errors preventing submission of the chart will be highlighted in the box under Validation Results on the Code Summary screen. Validation Results within the chart that should be reviewed and validated before the chart is finalized and submitted for billing.
ERROR results will display in RED
. These are hard stops that will prevent the chart from being submitted. The Submit button will be grayed out until errors have been resolved, including pending reasons that have been assigned.
Warning results will display in YELLOW
. These are reminders/suggestions for the user. Warnings do not need to be resolved before submitting the chart.
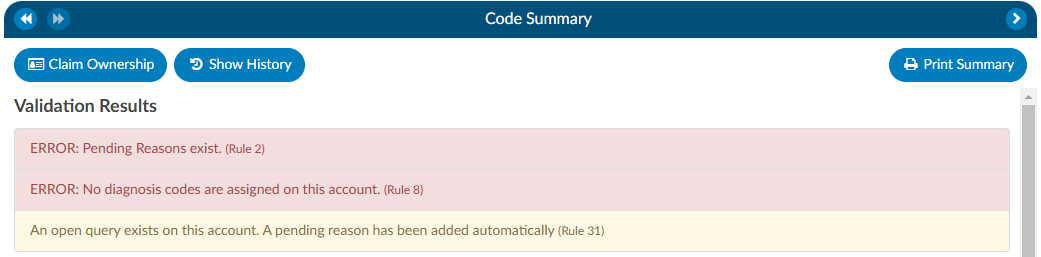
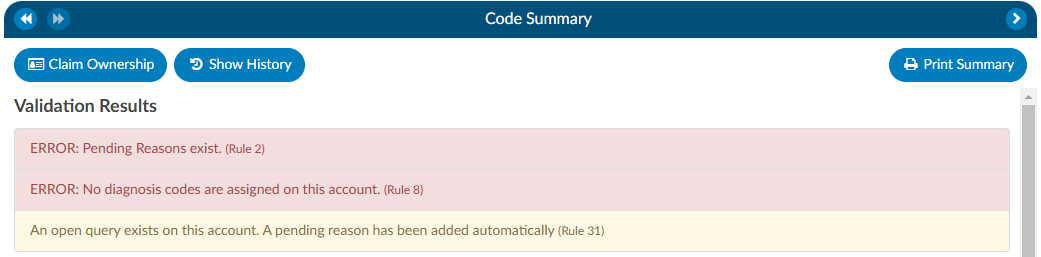
Once all necessary validations results are resolved, the Code Summary link in the Navigation tree will return to black and users can hit the Submit button to complete the chart.
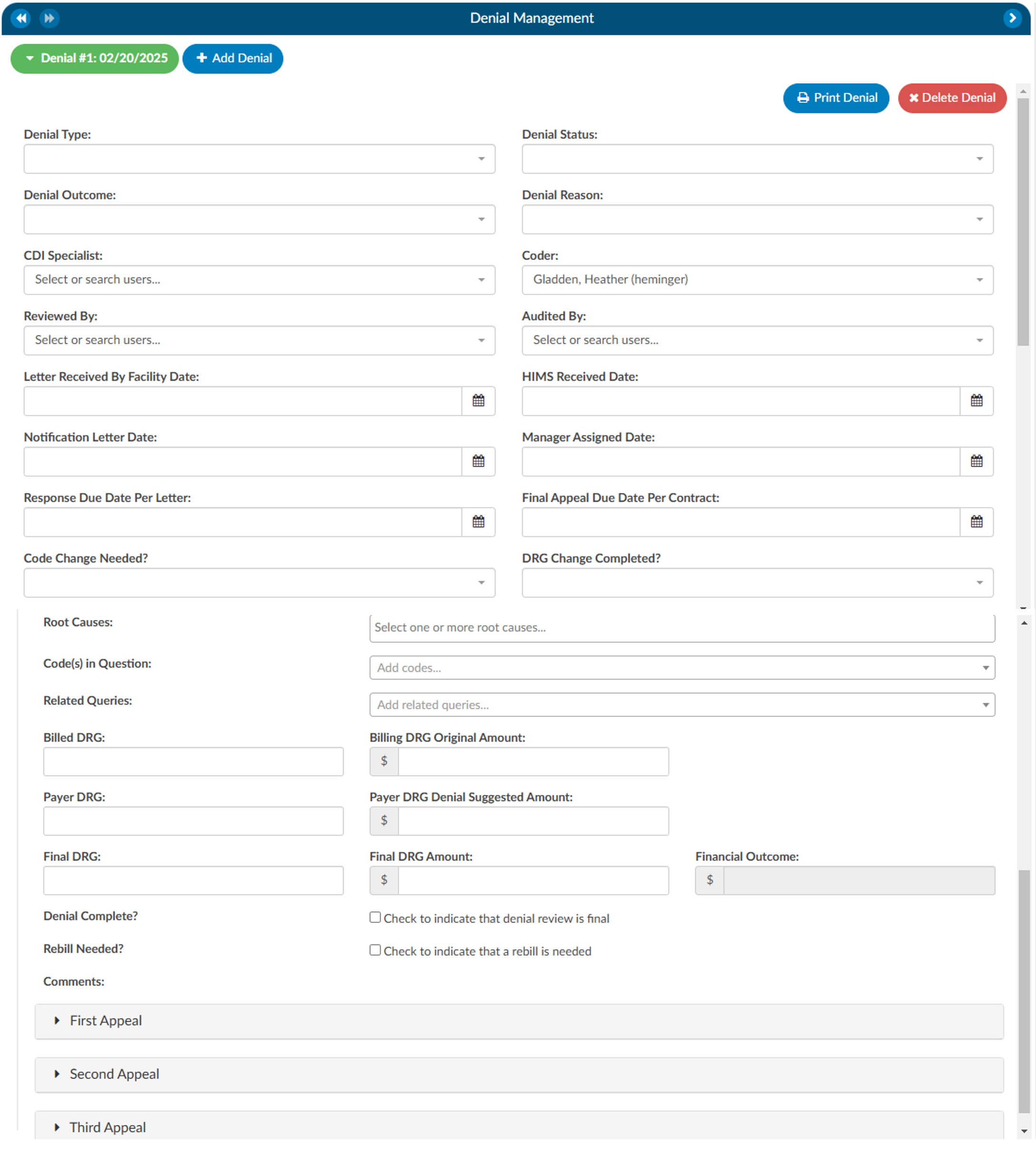
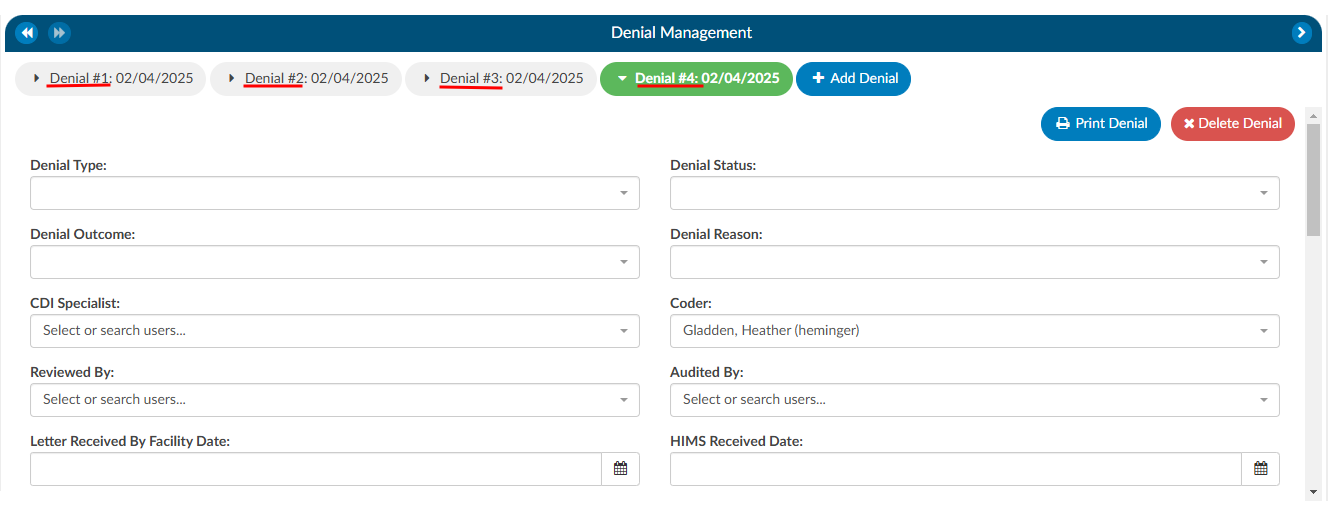
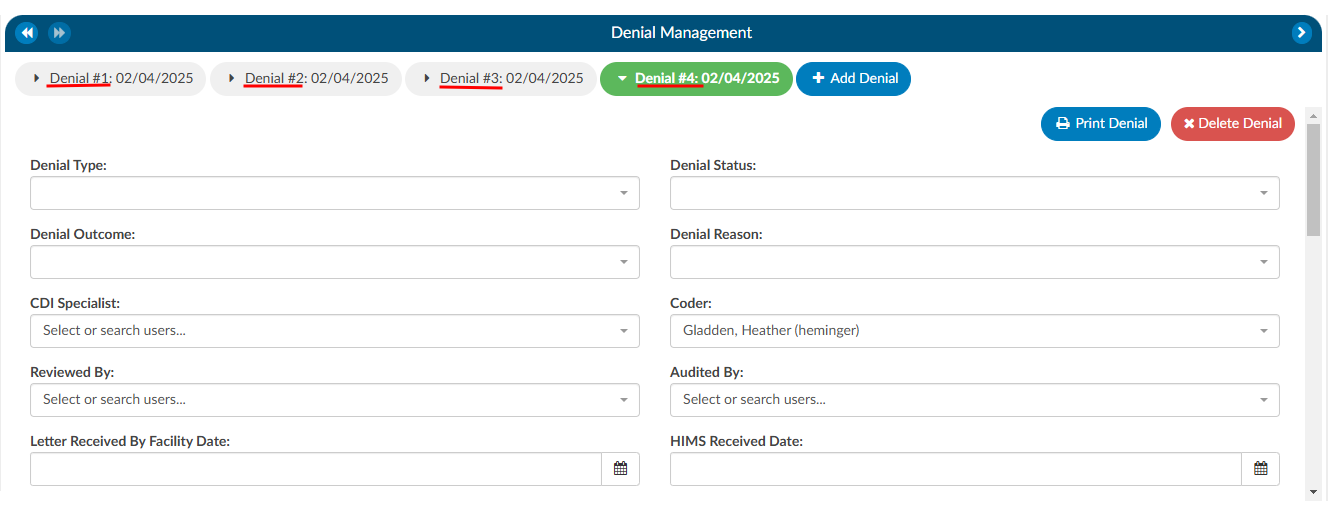
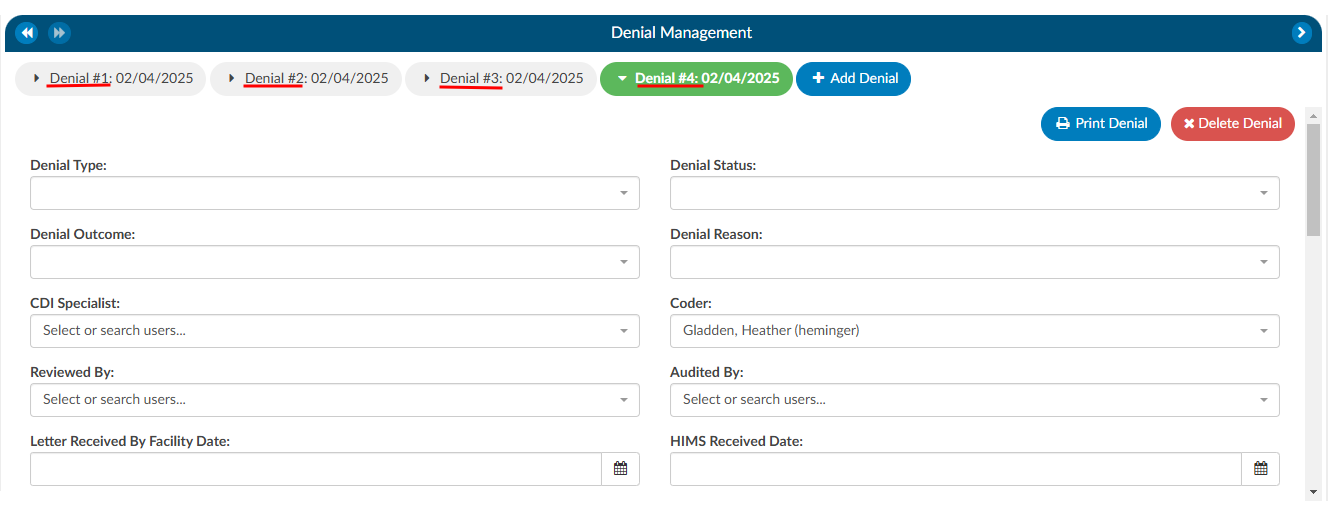
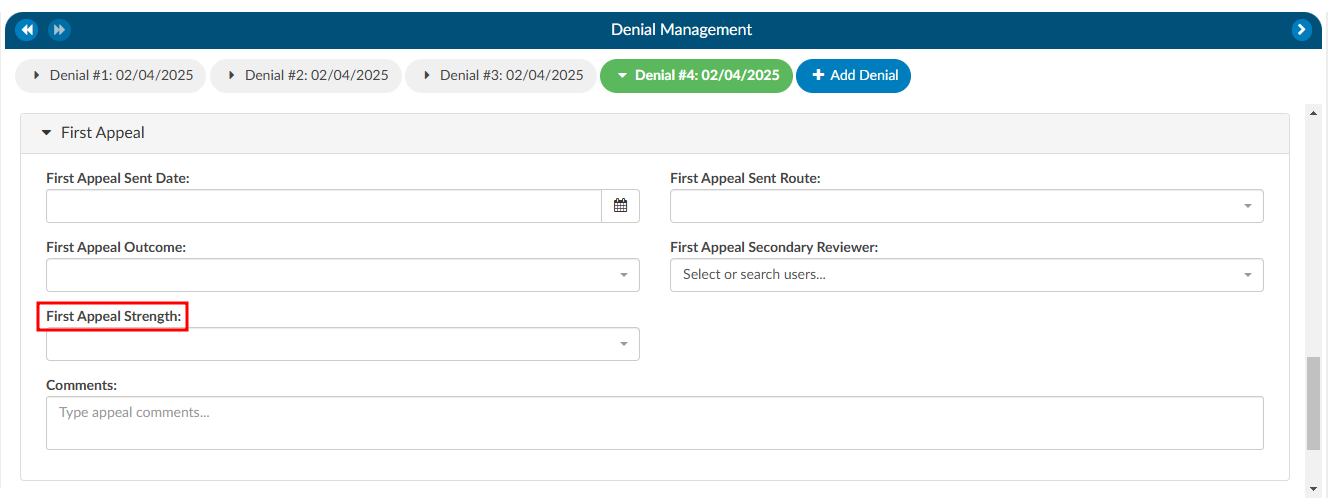
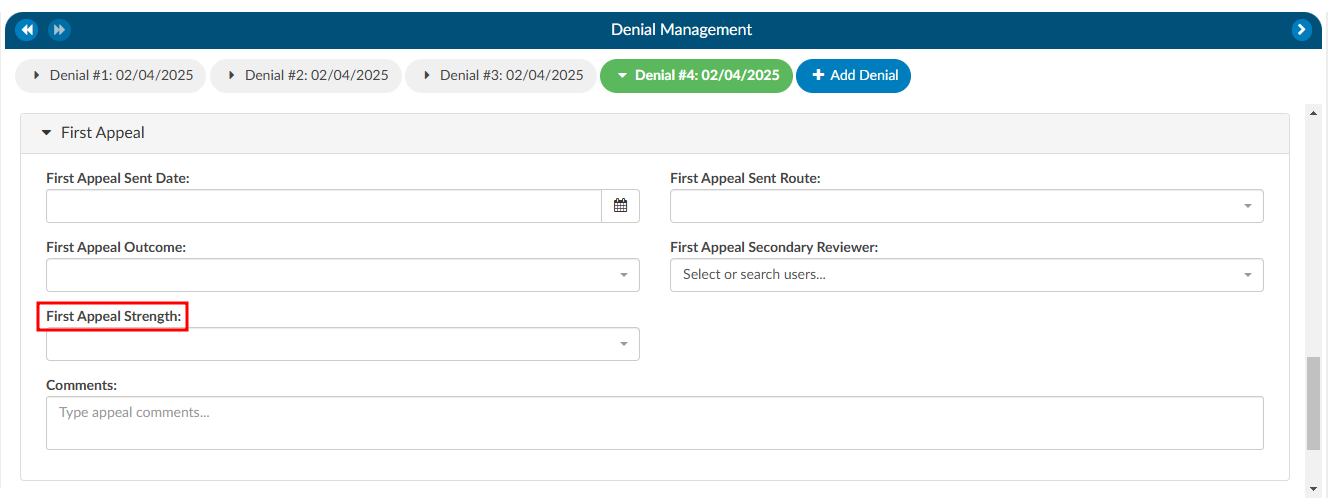
Denial Management
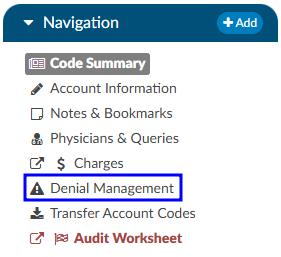
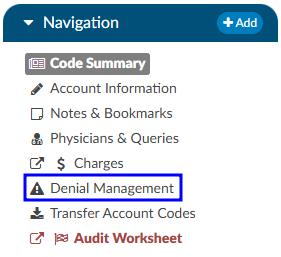
The denial management viewer displays on submitted accounts. Clicking on this viewer presents a form with several fields to be filled in when an account has been denied payment.
Denial management tracking involves monitoring cases where a patient’s submitted billing chart is rejected by the payer. Various reasons, such as medical necessity, code, or DRG assignment, could lead to these denials. This tool is designed to comprehensively record the specifics related to denial management and tracking. It is capable of documenting multiple denials for each chart, with the ability to log and categorize them for the purpose of tracking, managing workflows, and generating reports.
Adding a Denial
To add a denial, select “Denial Management” in the Navigation tree. This option will only be available if the account has been submitted. This will open up the Denial Management viewer in the center of the screen to then click on the +Add Denial button.


Once a denial has been added, a form with multiple fileds will need to be filled in by the user working the denial. The fields are made up of various drop-down options, dates, and financial information about the denial.
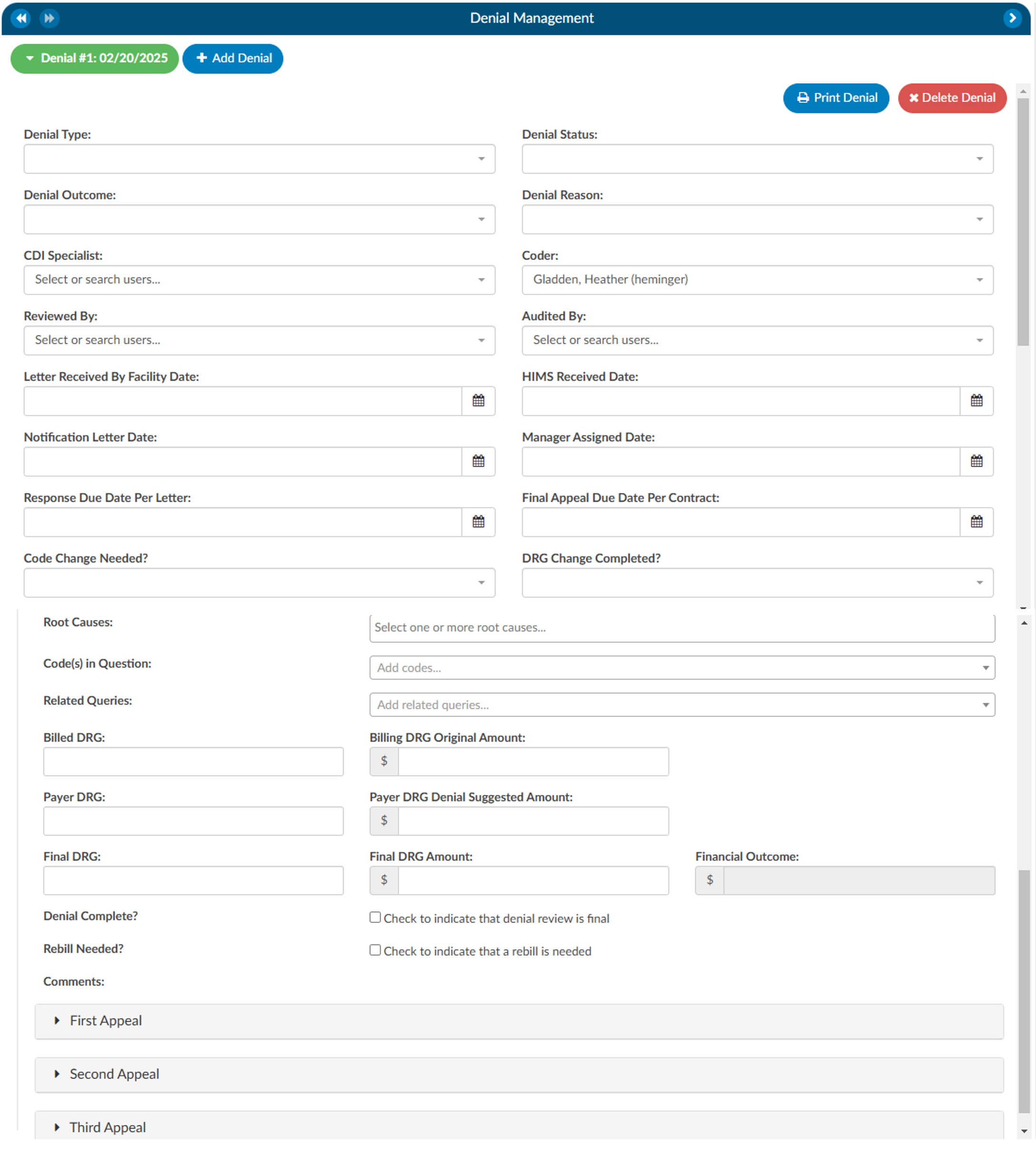
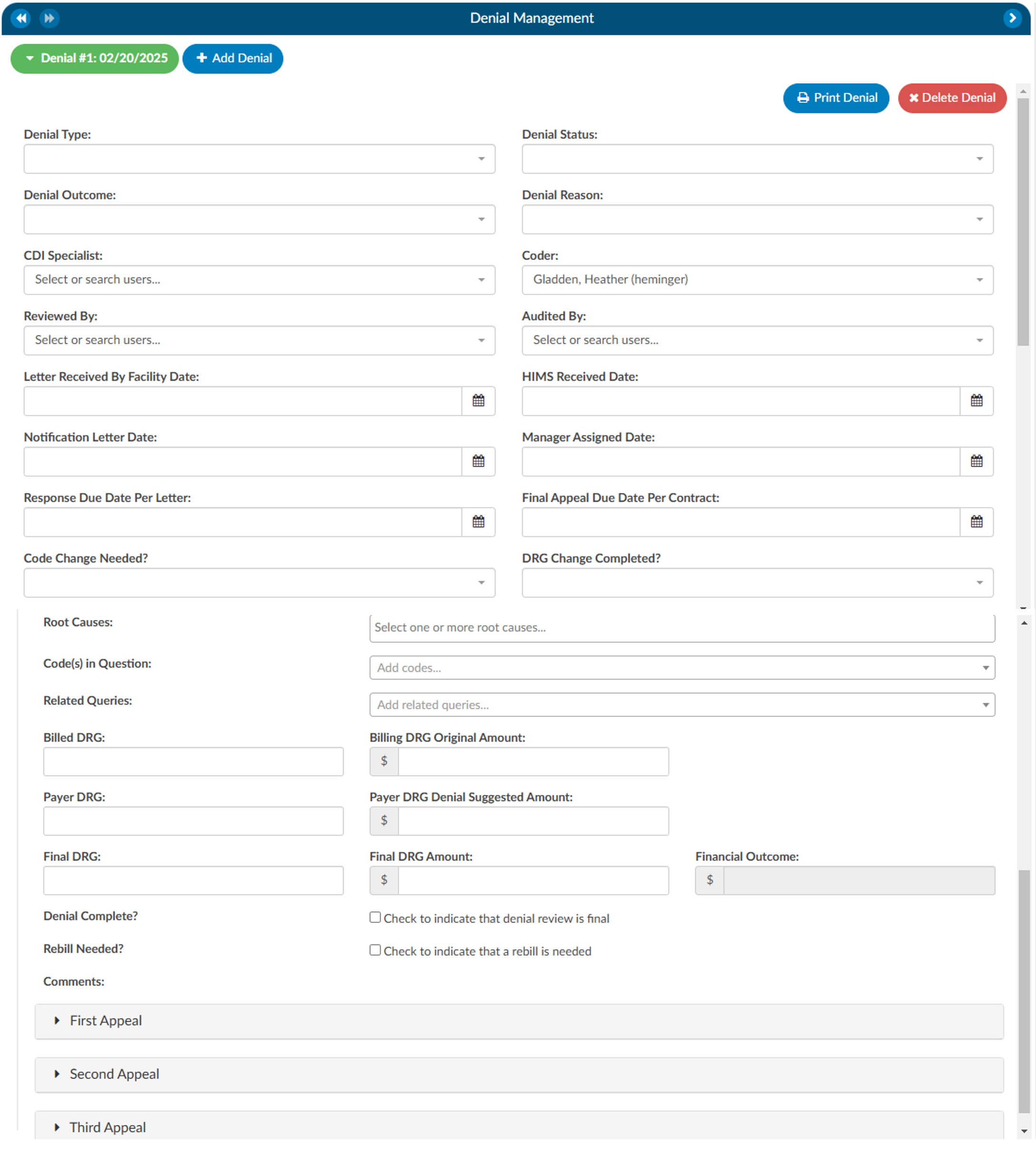
Auto-populated Fields
The Coder Field will be defaulted to the Owner of the account as long as it is not a CDI Specialist. If there is no Coder but a Submitter, the field will default to the Submitter. If there is no Owner, the field will be left blank for user input.
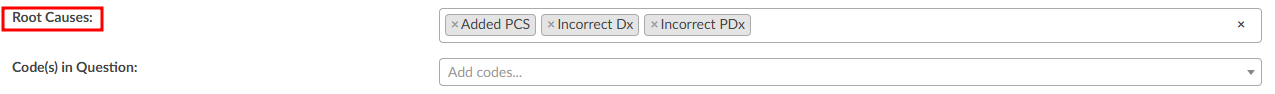
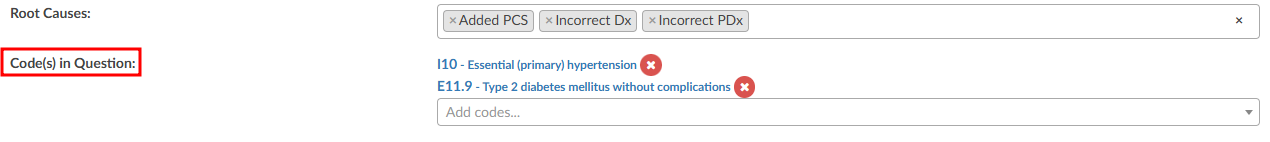
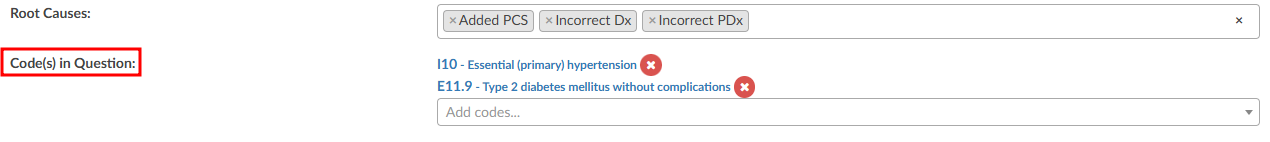
The Root Cause field has a drop down of options where one or more options can be selected.
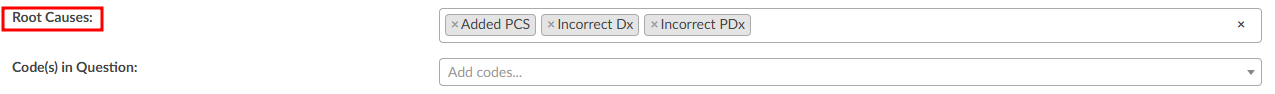
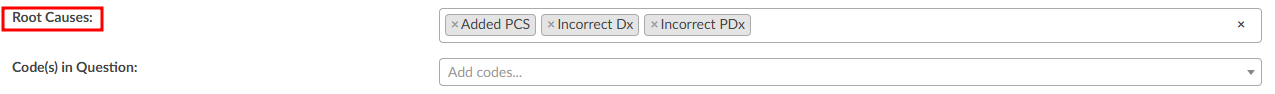
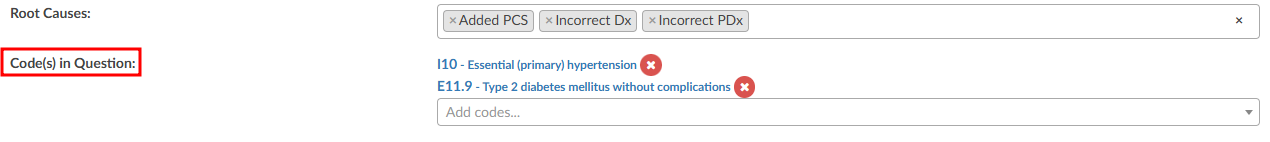
There can also be multiple Code(s) in Question entered.
Options in the fields above with dropdown lists can be customized per organization by editing the appropriate mapping table in Mapping Configuration. These fields include the following:
- DenialType
- DenialStatus
- DenialOutcome
- DenialAppealRoute
- DenialReason
- DenialCodeChangeNeeded
- DenialDRGChangeNeeded
- DenialRootCauses
Each field (except Comments) can be added to Grid Column Configuration for display in Account Search. These fields can also be used in workflow if necessary.
As needed, mutiple denial sheets can be created for a single account. To do this, click on the +Add Denial button. As more denials are added to an account, they will be listed at the top of the Denial Management viewer. The denial a user is working on will be indicated in green bubble.
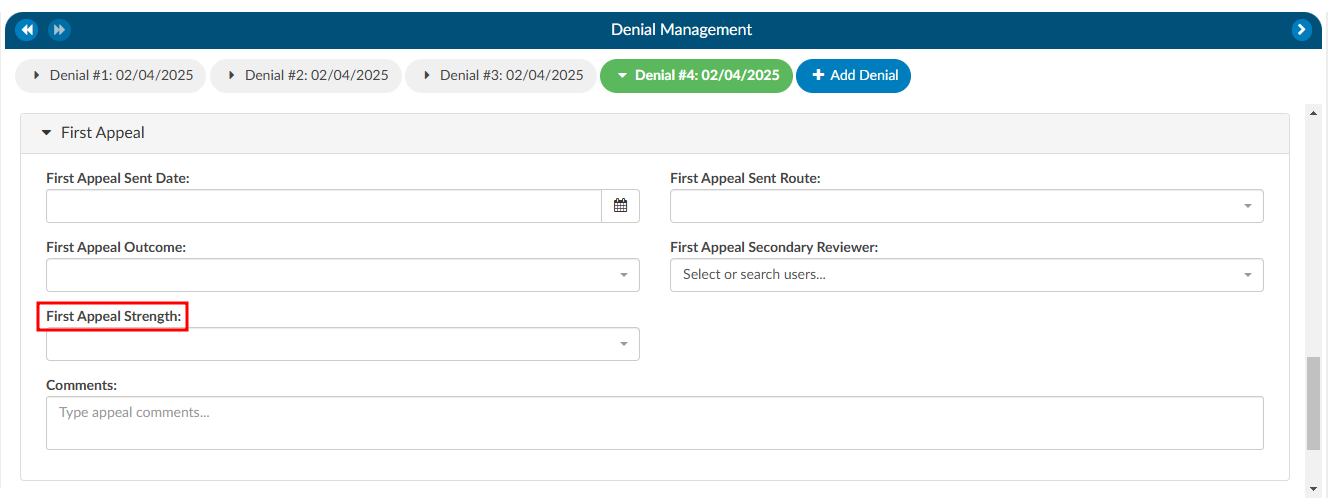
Appealing a Denial
If a denial needs to be appealed, there are separate fileds to track when those appeals were sent, how it was sent, and the outcome of the appeal. A user can track the strength of the appeal as low, medium, and high based on their organizations preferences. Additionally, a comment section has been added for any free text the user would like to enter.
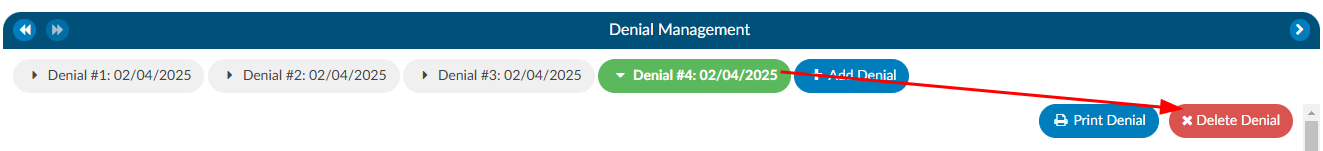
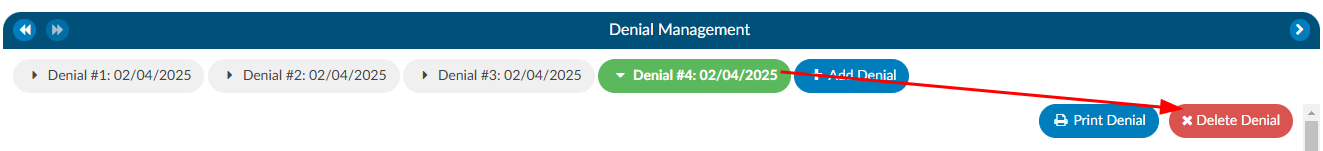
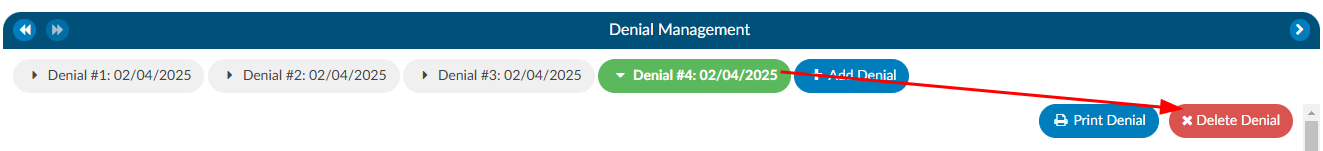
Deleting a Denial
If a denial needs to be deleted from the account, click on the denial the user wishes to remove, which will bee in the green bubble, then click on the xDelete Denial button.
Reporting Denials
For reporting within Account Search, a Denials drilldown is available. This drilldown only reports on the first denial on the account.
Documentation Reviews
The Documentation Reviewss module is designed to provide flexibility for sites that prefer a different style of Clinical Documentation Improvement (CDI) reviews or need alternative methods for tracking management reporting. This module allows users to customize and monitor documentation reviews by various topics and types. It is particularly useful when reviews do not fit the conventional workflows of initial, follow-up, or reconciliation reviews, such as for utilization management purposes.
Why Use Documentation Reviews?
Sites sometimes choose to add documentation reviews because reporting productivity is more complex than tracking initial, follow-up, or reconciliation reviews. The module’s flexibility allows CDI teams to capture and track additional review types that are essential for comprehensive reporting but might not fit within the standard review categories.
Standard Review Definitions
Before exploring the customization capabilities of the Documentation Review module, it is essential to understand the baseline definitions of reviews in a CDI system:
Review: A review is defined as a save on an account by a CDI Specialist (CDS) on a single day. For inpatient accounts, the specialist must also calculate a Working DRG. Multiple saves on the same account by the same CDS within the same day count as one (1) review. In other words, there can be only one review per account per CDS per day.
Initial Review: The first review saved on an account by a CDs. For inpatient accounts, the CDS must calculate a Working DRG for it to count as an initial review. There can only be one initial review per account.
Follow-up Review: A review saved on an account by either the same or a different CDS on a different day, following the initial review. No account will have more than one follow-up review per day for the same CDSS.
Example:
Day 1: CDI Specialist “A” saves an inpatient account with a Working DRG.
Day 1: CDI Specialist “A” updates the Working DRG (does not count as a separate review since it is within the same day).
Day 2: CDI Specialist “B” saves the account with the same Working DRG (counts as a follow-up review).
Day 3: CDI Specialist “A” saves the account with the same Working DRG.
Day 3: CDI Specialist “B” saves the account with a different Working DRG (counts as a follow-up review).
In this scenario, there is one initial review and three follow-up reviews. The change made by CDI Specialist “A” on Day 1 does not count as a follow-up because it occurred on the same day as the initial review.
Customizing Documentation Reviews
By default, the Documentation Review module includes a free-form text field, allowing CDI specialists to capture detailed information about their reviews. However, sites can further customize the module by creating forms specific to different review types, enabling more structured and consistent data entry.
Using the Worksheet Designer, sites can create tailored forms for different documentation review types. These forms can help standardize data collection and improve reporting accuracy. Some common examples of custom review types include:
- MD Advisor Response
- Query Opportunity Reply
- Coder Question Response
- Post-Discharge Follow-up
- Pre-Bill Review
- Retrospective Query Needed
- Query Review
- Case Management Review
- Quality Improvement (QI) Review
- Utilization Review
- Types of Reviews
Custom reviews allow CDI teams to track reviews that fall outside of traditional CDI workflows. These reviews can be particularly useful for:
- Post-Discharge and Pre-Bill Reviews: These reviews focus on ensuring documentation accuracy and completeness before the billing process, helping to reduce denials and optimize revenue capture.
- Query and Retrospective Reviews: These reviews allow CDI teams to capture follow-up actions taken after initial queries or when additional queries are required after discharge outside of a traditional review.
- Utilization Management Reviews: These reviews may not fit into the standard initial or follow-up workflows but are crucial for tracking how effectively hospital resources are used and ensuring proper reimbursement.
- Reporting and Productivity: Tracking productivity for non-standard reviews (such as utilization reviews or post-discharge follow-ups) can be more complex than traditional reviews. Customizing the module allows sites to generate more meaningful reports that reflect the variety of documentation efforts made by CDI teams.
In the CDI Summary section of the dashboard, counts of reviews are displayed, such as “In the Last 7 Days,” excluding the current day. This allows for real-time tracking of CDI efforts and helps managers assess team productivity.
CDI Productivity by Review Type
This report shows productivity by each user by custom documentation review type.
CDI Detailed by Review
This report provides details about the custom documentation review type of CDI reviews performed by account.
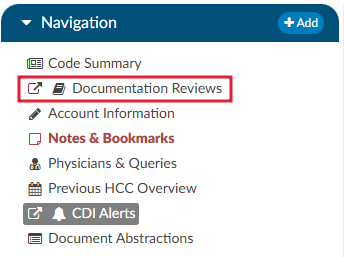
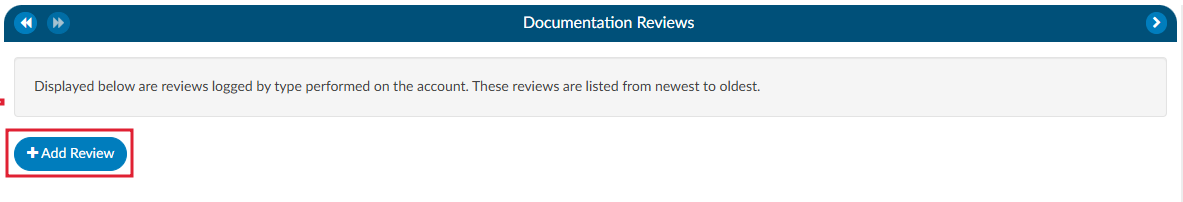
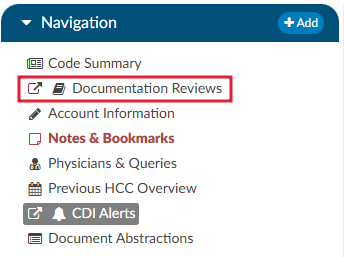
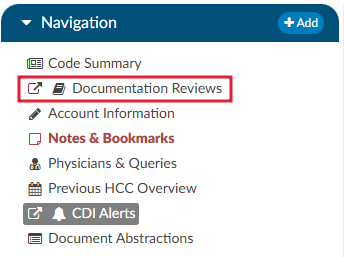
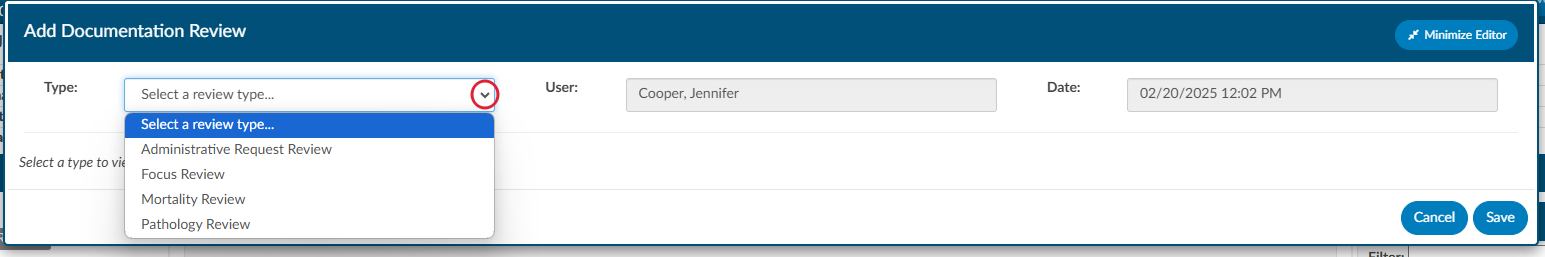
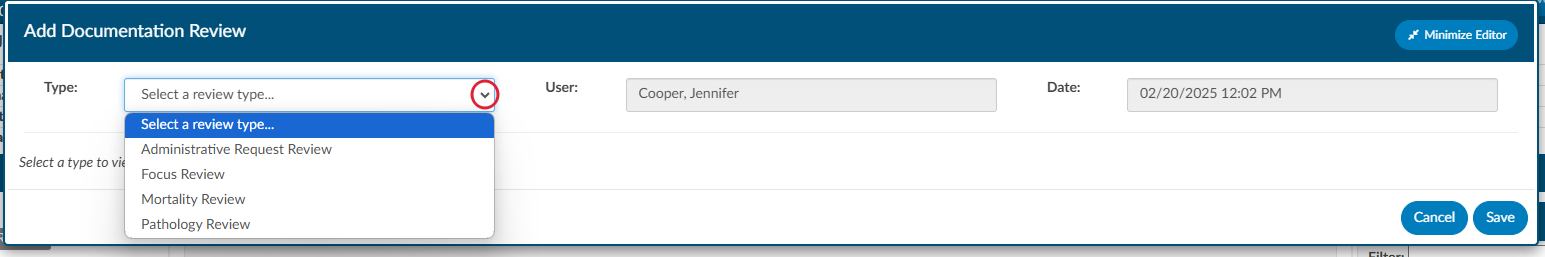
Navigating to Documentation Reviewss
Unlike the CDI Worksheet which is located under the Document tree, the Documentation Reviewss section is found on the Navigation tree within the user interface. This distinction allows easy access to reviews that are separate from the standard CDI workflows and documents.
Steps to Access Documentation Reviews
- Locate the Navigation tree: Once logged into the system, navigate to the left-hand side of the screen where the Navigation tree is displayed.
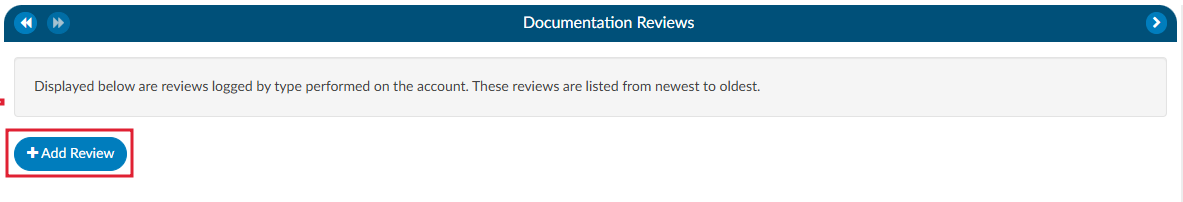
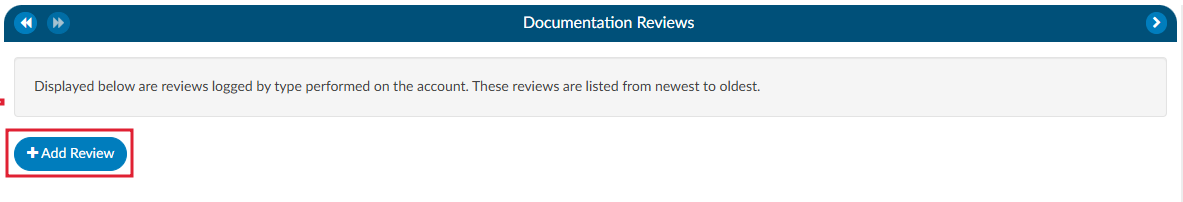
- Select Documentation Review: Under the Navigation tree, will be the Documentation Reviews section. Click on it to open the review interface.
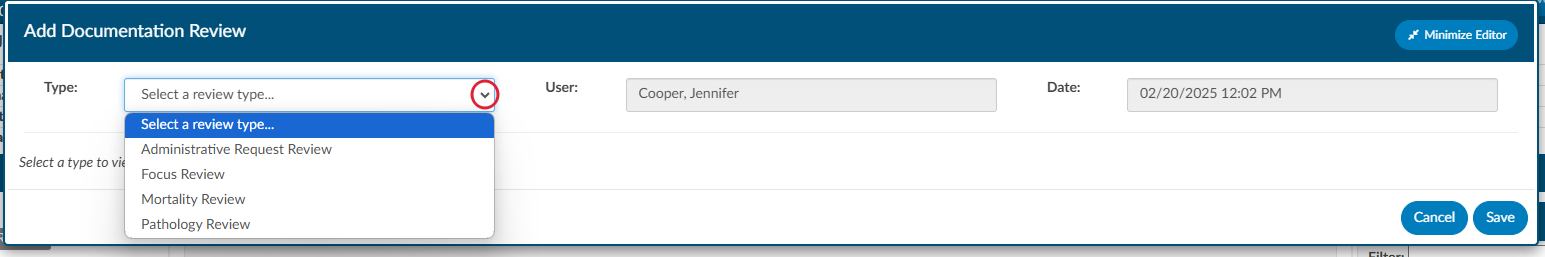
- Adding a New Review: Upon opening the Documentation Reviews viewer, there will be the option to +Add Review. This allows the user to select the specific review type from the list of available choices. The choices available are customized per organization and can include any form types an organization has designed.
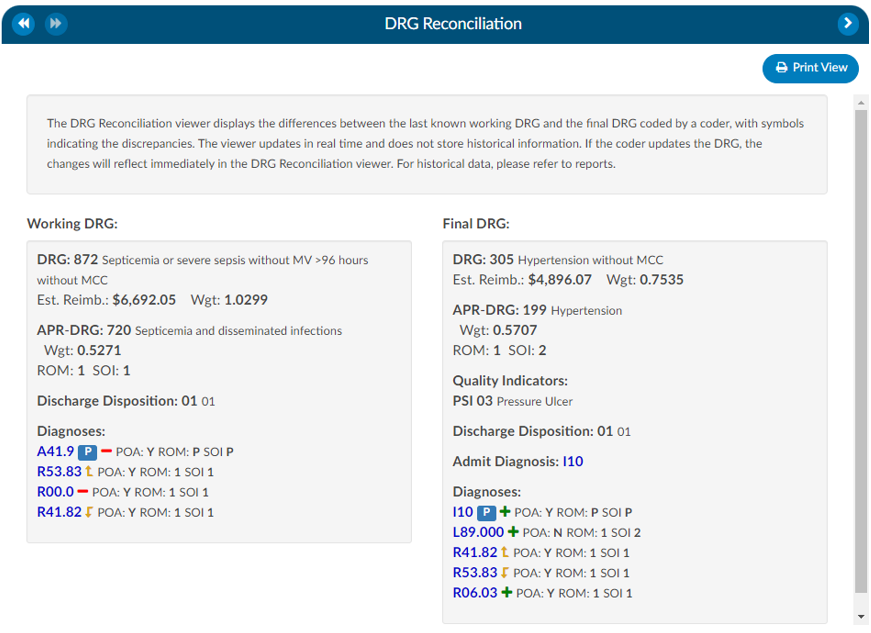
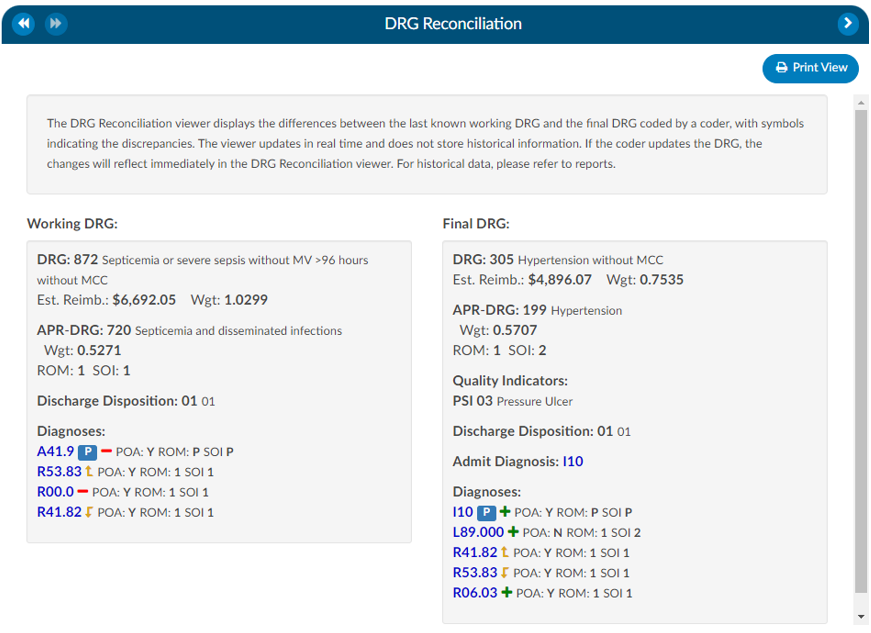
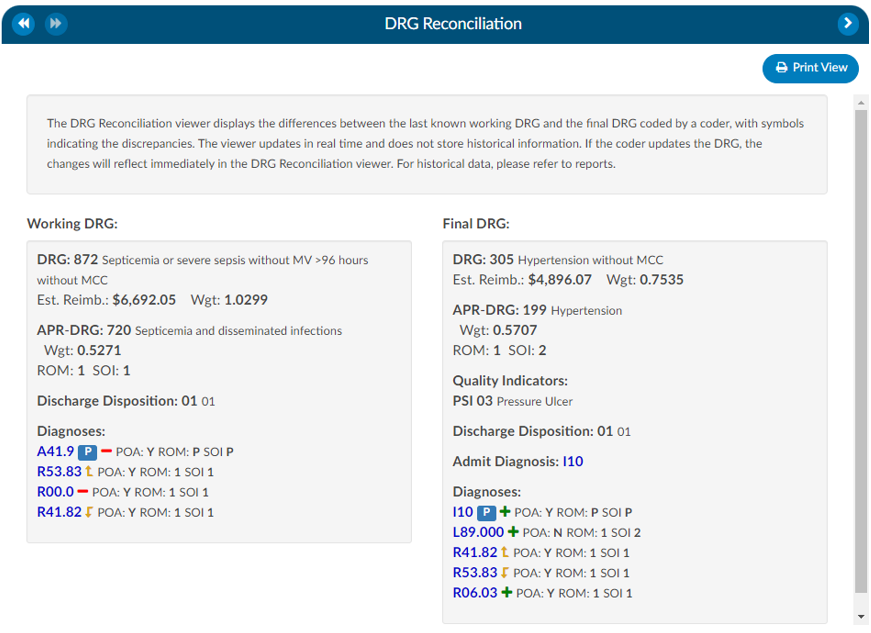
DRG Reconciliation
The DRG Reconciliation viewer displays the differences between the last known Working DRG and the Final DRG coded by a Coder, with symbols indicating the discrepancies. The viewer updates in real time and does not store historical information. If the Coder updates the DRG, the changes will reflect immediately in the DRG Reconciliation viewer. For historical data, please refer to reports.
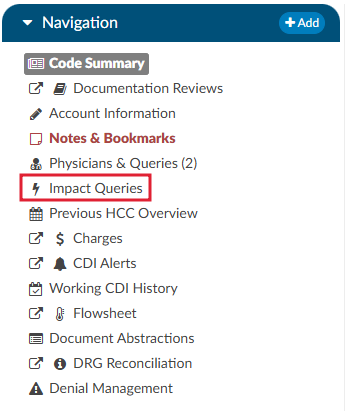
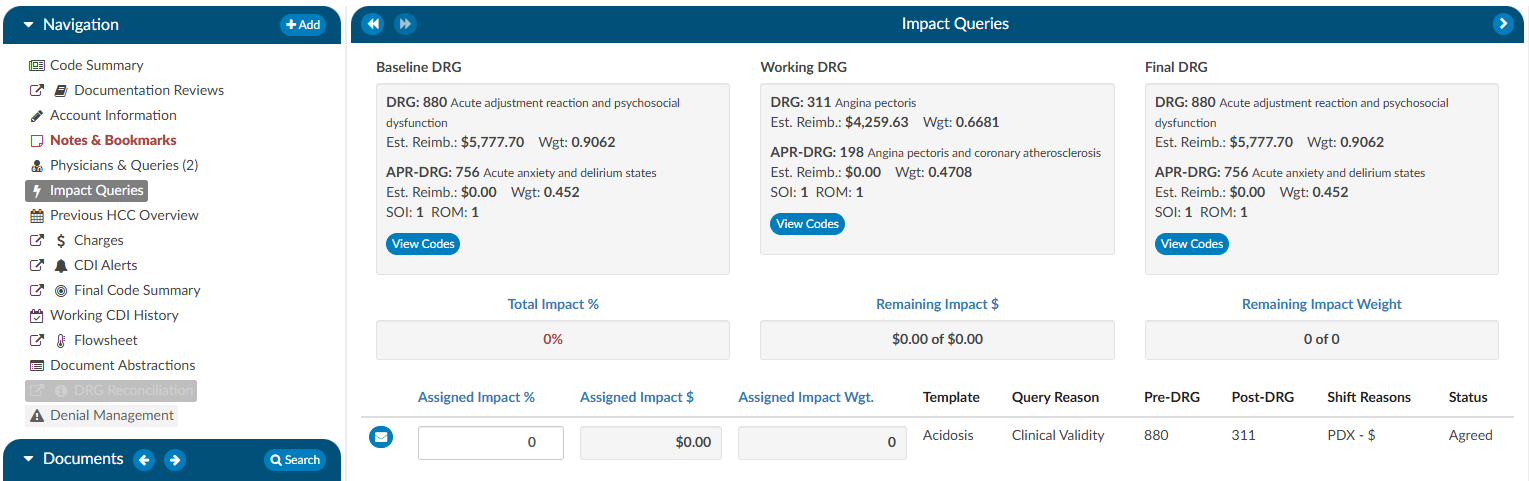
Impact Queries
The Impact Queries Viewer is designed exclusively for CDI teams. This tool may not be necessary for all customers, but it serves a specific purpose for those who use it. CDI teams often issue multiple queries per account and require a way to track the impact of each query distinctly. This viewer allows teams to determine whether the impact of a query accounts for the total change in the account or if it shares this impact with other queries.
Purpose and Use
- Impact Tracking: Allows CDI specialists to clearly see the account impact of each query, from the initial baseline to the final assessment after all queries.
- Impact Assignment: Within each query, CDI specialists can assign a percentage to quantify the impact of the query on the account. This percentage is then translated into a dollar value attributed to the query.
This feature helps prevent double-counting and overestimating the impact that CDI claims on an account. After coding is completed, CDI specialists must revisit and reassess the account to determine and specify the precise impact each query had.
By using the Impact Queries Viewer, CDI teams can ensure more accurate and accountable query impact assessments, contributing to more precise documentation and reimbursement processes.
To access the Impact Queries Viewer, the user must have a CDI role AND there must be at least one (1) query sent by a CDI user.
Displayed at the top of the viewer is the Baseline, Working and Final DRG. The account impact equals Final DRG – Baseline DRG.
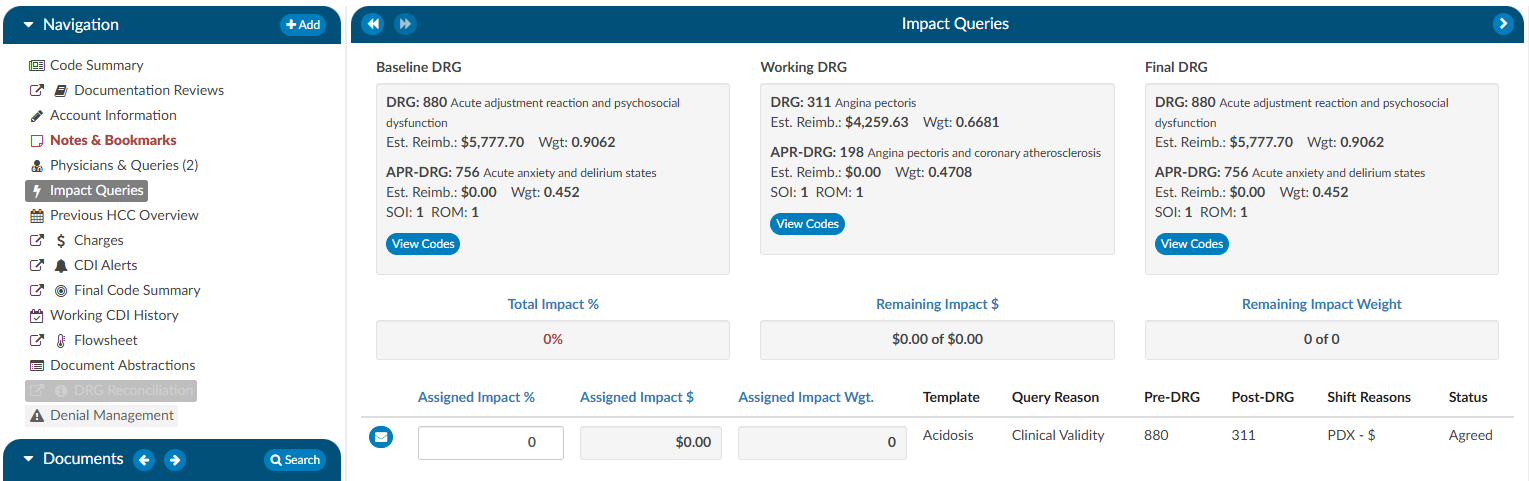
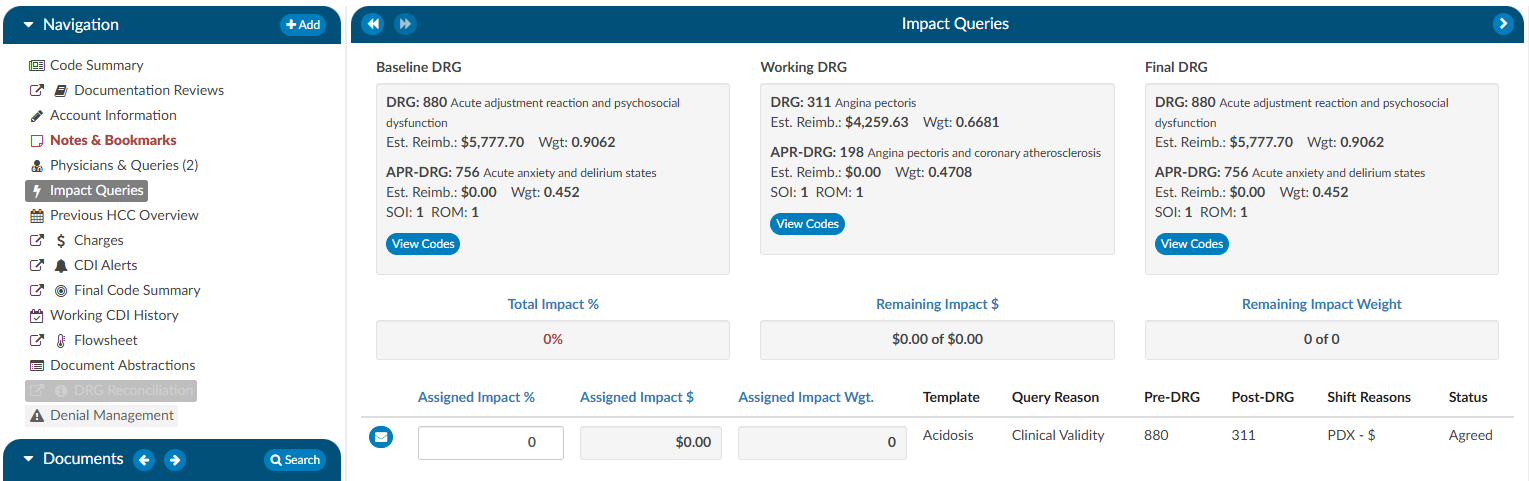
Clicking on the View Codes button in either the Baseline or Working DRG boxes will take the user to the Working CDI History viewer to allow the user to view how the CDS developed their DRG at different stages. Clicking on the View Codes button in the Final DRG box will take the user to the Final Code Summary viewer to show the user how the account was final coded by the Coder.
To review the query that was assigned, click on the BLUE ENVELOPE
. This will open the query in a dialouge box.
To assign the impact of the query, the user will enter a percentage in the “Assigned Impact %” field. This will autocalculate the following fileds:
- Total Impact %
- Remaining Impact $
- Remaining Impact Weight
- Assigned Impact &
- Assigned Impact Wgt.
| Field | Definition |
|---|
| Total Impact % | This the % of the impact assigned to queries it can never exceed 100% but, it is allowed to be less than 100%. The impact % must be assigned in the assigned impact % field per each query. |
| Remaining Impact $ | This is the account impact dollars left to divy out. Think about this like a bank account if the account impact between the baseline and final DRG is $10,000 it should start off with $10,000 then if we assign 50% of the account impact to the first query then it would reduce to $5k and so on. |
| Remaining Impact Weight | This is the same concept as Remaining Impact $ we have a field for Remaining impact weight since some sites do not have reimbursement dollars in the system. |
| Assigned Impact % | This is the % of the account impact you are assigning per query. |
| Assigned Impact $ | This is the $ of the account impact you are assigning per query based upon the % you placed in the assigned impact % field that pulls from the remaining impact $. |
| Assigned Impact Wgt. | This is the weight of the account impact you are assigning per query based upon the % you placed in the assigned impact % field that pulls from the remaining impact weight. |
| Template | This is the query template you are assigning impact to. Only queries issues by CDI will display here. |
| Query Reason | This is the query reason to assigned to the query template. |
| Pre-Drg | This is the pre-DRG assigned to the query, to change this click on the blue envelop icon to the right of assigned impact. |
| Post-Drg | This is the post-DRG assigned to the query, to change this click on the blue envelop icon to the right of assigned impact. |
| Shift Reasons | This is the shift reasons assigned to the query, to change this click on the blue envelop icon to the right of assigned impact. |
| Status | This is the status of the query, to change this click on the blue envelop icon to the right of assigned impact. |
Impact Assignment
For guidelines on how to quantify the impact of a query, or queries, Users should contact their supervisor for any internal policies and procedures.
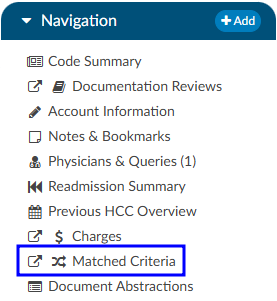
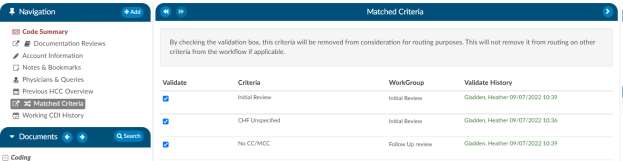
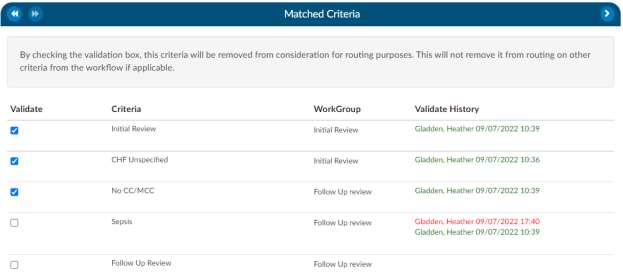
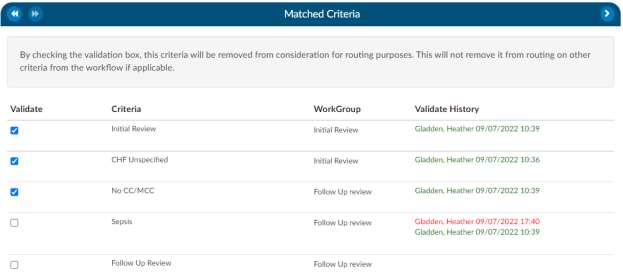
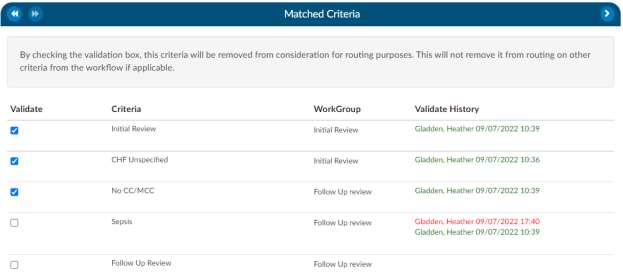
Matched Criteria
CDI Users Only
The Matched Criteria viewer is only visible if the active role is CDI Specialist.
The Matched Criteria viewer allows a user to see why the chart was routed to them. The matched criteria group is a list
of “Criteria Group” that the chart matched upon when it went through workflow. These criteria groups
are used to indicate a “possible” query opportunity based upon the criteria outlined in workflow.
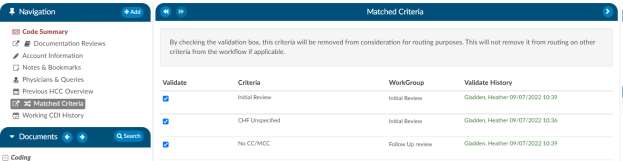
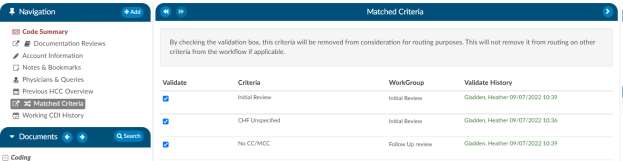
Prioritizing Workflow using Matched Criteria
Matched Criteria can be used to prioritize workflow using one of two fields:
Criteria Group - This field will tell the name of the criteria that the workflow routed the
chart to the CDI users. Often times the field is renamed to “Routed Reason” because this field represents
why the chart was routed to the user. If the chart matches multiple criteria groups the criteria group
that is displayed in this field is the first one that it matched. All others that it matched with will
display within the Matched Criteria viewer when the chart is opened.
Active Matched Criteria Groups - This is often renamed as “Opportunities” and is defined as the number of matched criteria groups the chart matched with, which reflects the total number of possible query opportunities currently present on the patient chart. This field can be used by the CDI user to sort the worklist based upon the charts that have the most to least possible query opportunities.
Once a CDI user validates a criteria group by checking the box next to its name in the Matched Criteria viewer, that criterion is removed from consideration for routing purposes. However, this does not affect other criteria that may still be active in the workflow.
If multiple worklists contain the same matched criteria group names and a chart has already had a prior matched criteria group with the same name validated, it will not be retriggered or displayed in the Matched Criteria viewer.
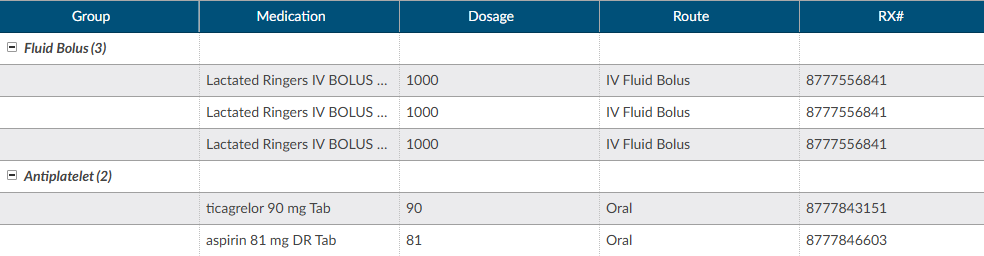
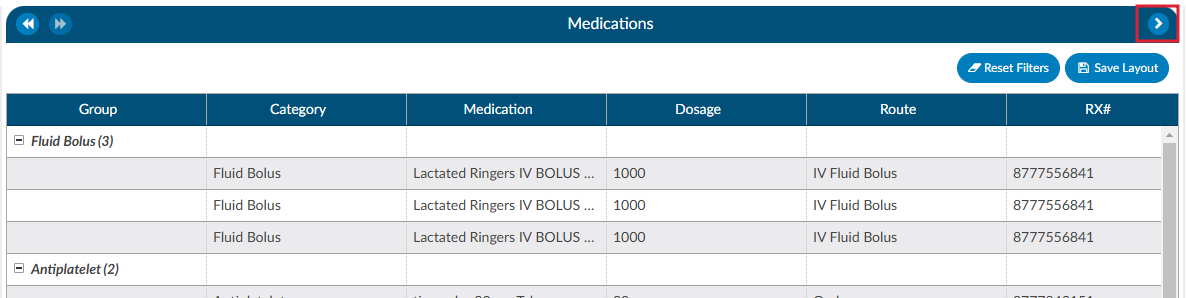
Medications
A Medication Administration Record (MAR, or eMAR for electronic versions), commonly referred to as a drug chart, is the report that serves as a legal record of the drugs administered to a patient at a facility by a health care professional. The MAR is a part of a patient’s permanent record on their medical chart. The health care professional signs off on the record at the time that the drug or device is administered.
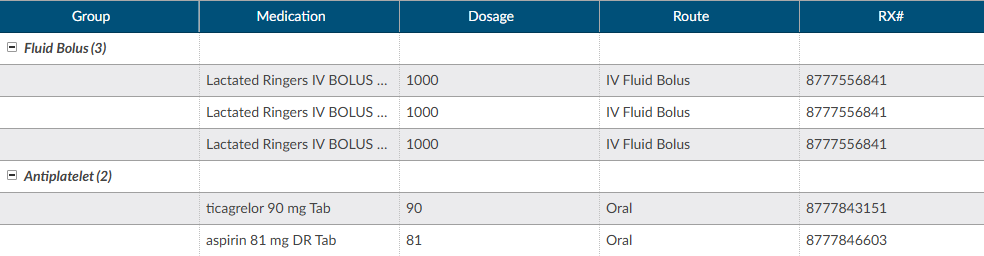
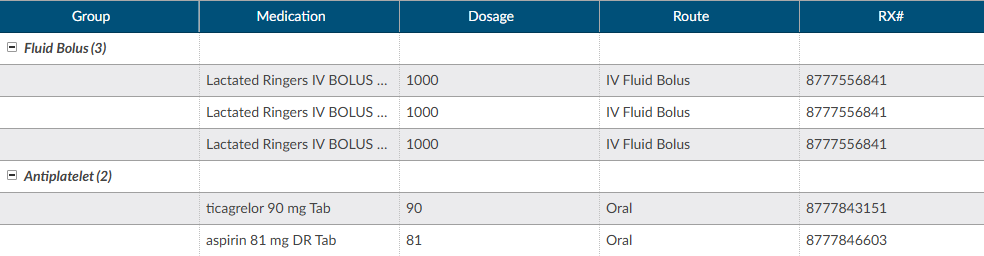
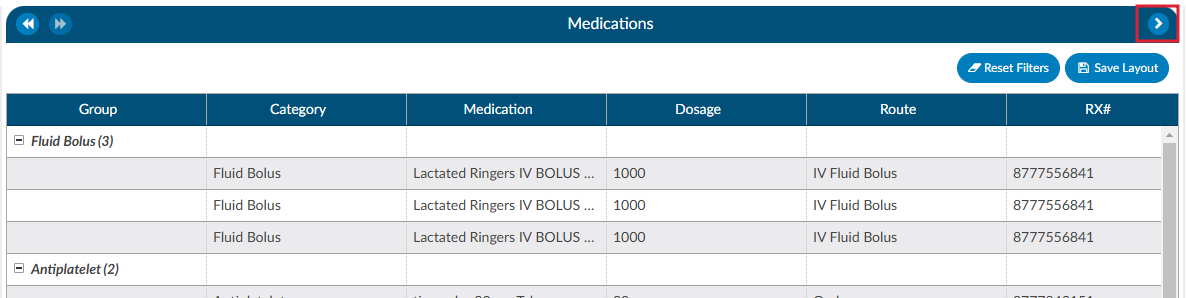
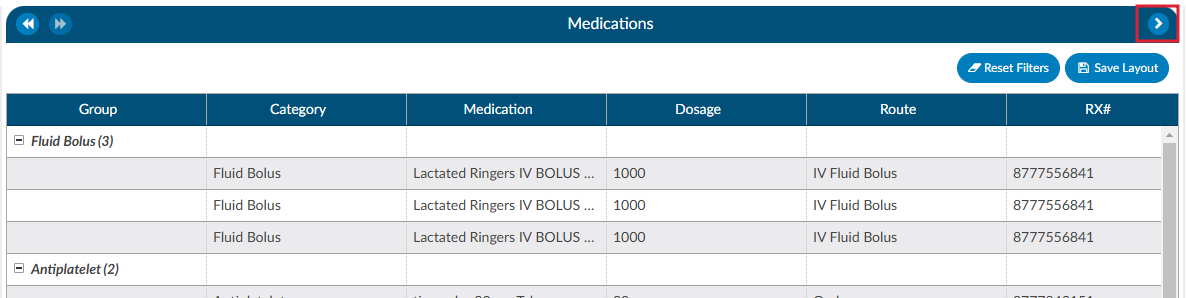
There are activity buttons to “Save Layout” or expand the Medications viewer. Users can expand the width of the Medications viewer to view more available columns by clicking on the arrow in the top right corner of the viewer. This viewer also provides columns that can be sorted or filtered based on the user’s need. The columns include the medication Group, Category, Medication name, Dosage, Route, Rx#, Start Date/Time, and End Date/Time.
Column Settings
Each column within the Medications grid has menu options to Pin Column, Autosize, and Reset Columns. Click on the Menu icon to view the drop-down listing. After making column setting selections, click on the button to retain column settings for future coding sessions.
| Column Setting | Definition |
|---|
| Pin Column | Allows users to select the column and then pin it to the RIGHT or LEFT side of the assigned accounts grid. This function works similarly to freezing columns in Excel. |
| Autosize This Column | Select this option to change the column width to automatically size the width of the column for contents of the cells in this column. |
| Autosize All Columns | To quickly autosize all columns in the assigned accounts grid, click the Autosize All Columns button. |
| Reset Columns | Click on this option to Reset Columns to their default column width. |
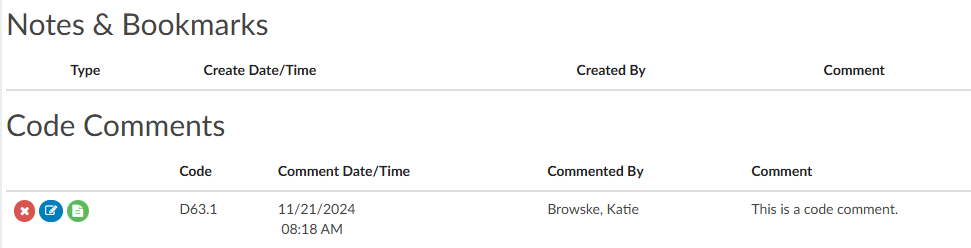
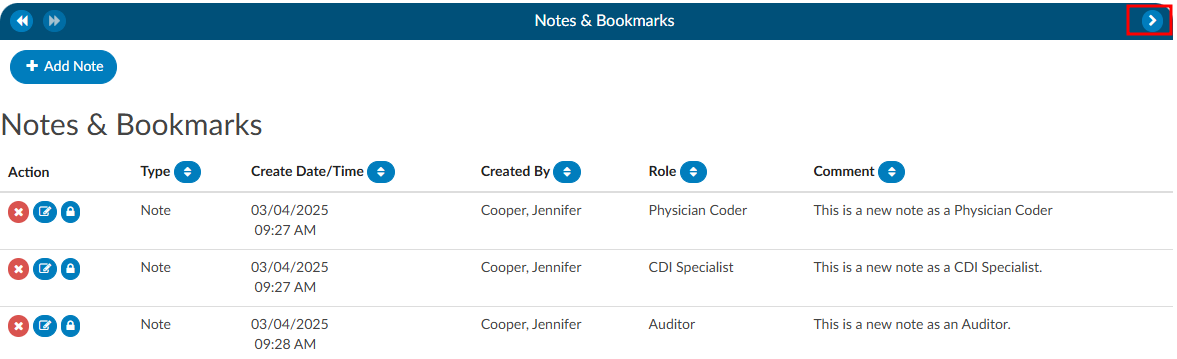
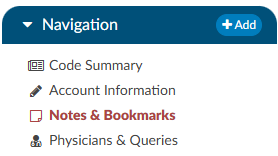
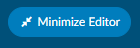
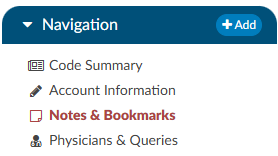
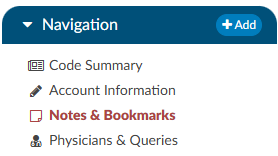
Notes & Bookmarks
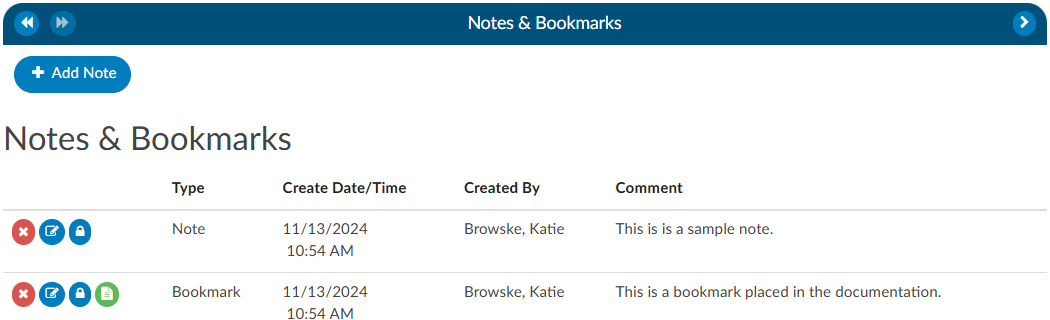
Notes & Bookmarks becomes visible in the center viewer after clicking on the hyperlink from the Navigation tree. This viewer presents a summary and chronological history of all notes and bookmarks added to an account. Users can expand the width of the Code Summary viewer by clicking on the arrow in the top right corner of the viewer.
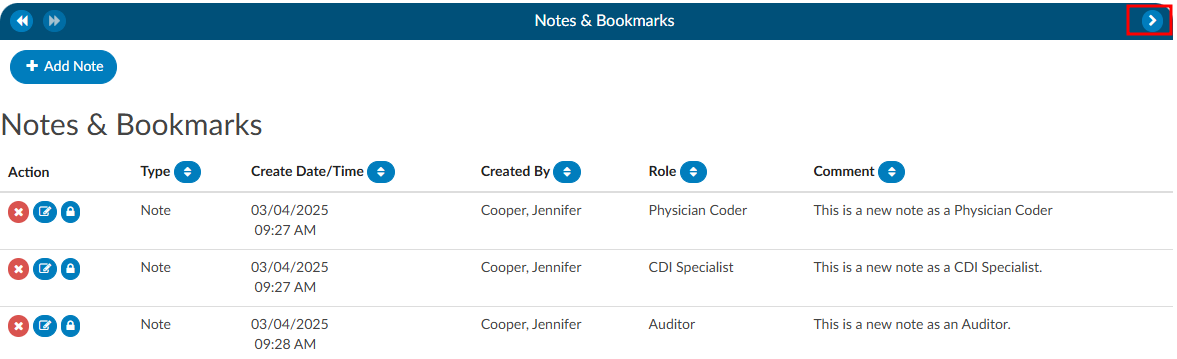
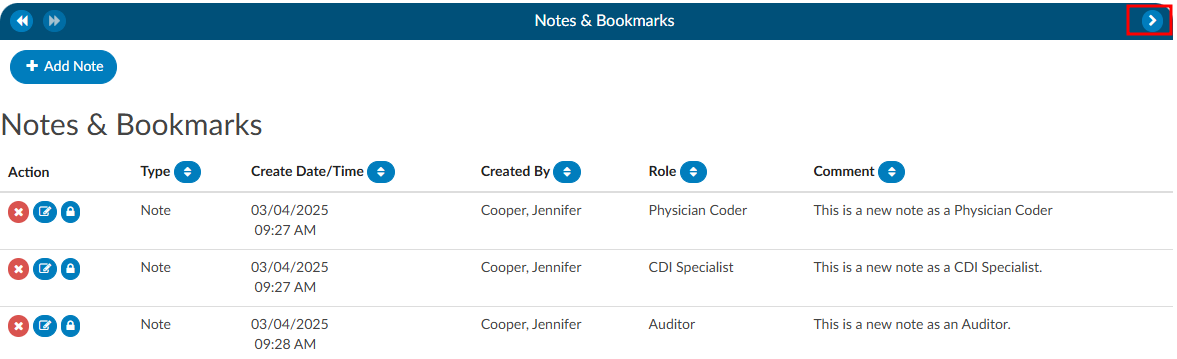
Notes
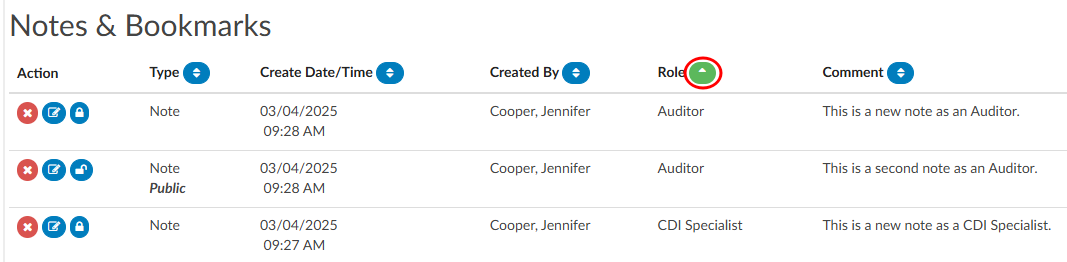
Notes can be added to the patient chart by clicking on the +Add Note button within the Notes & Bookmarks viewer.


When notes or bookmarks are applied to the chart, the Notes and Bookmarks link in the Navigation tree will turn red.
The columns in the Notes & Bookmarks viewer include the following:
- Action - Notes can be deleted, edited, or made private.
- Type - This will show if it is a Note or a Bookmark.
- Create Date/Time - This is a timestampe of when the Note or Bookmark was created.
- Created By - This shows the user’s name
- Role - This shows the user’s role, which will be the role they were logged in as when they made the note if they have multiple roles.
- Comment - This is the section where the user made the note.
The columns can be sorted in ascending or descending order. The column that is sorted will have a green arrow next to the column name. This is helpful if the user is looking for a note or bookmark by a specific date, user, or user role as an example.
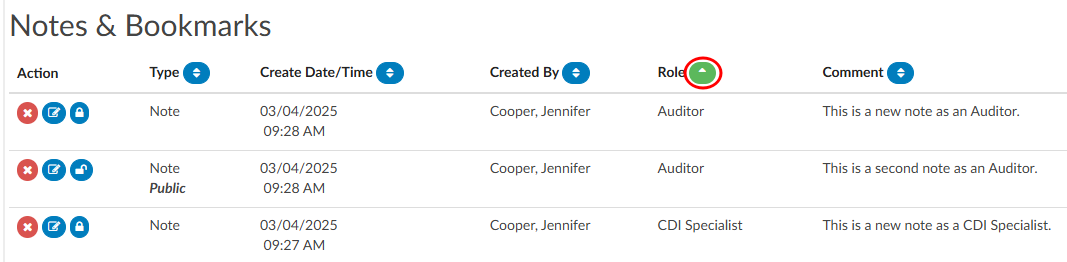
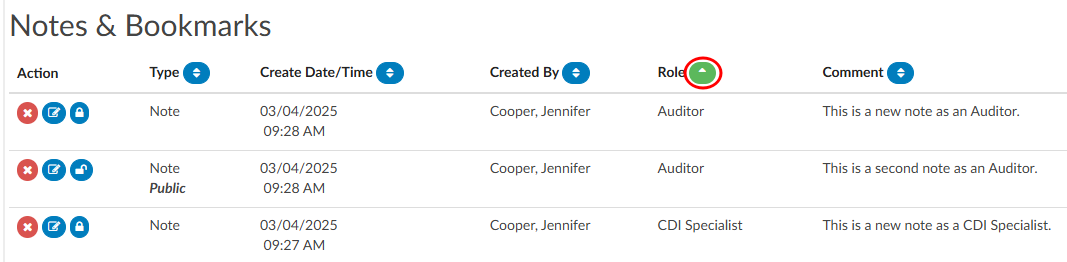
Account Notes also have formatting options for text. Highlighting the text displays a pop-up with formatting options. A user can now select text in those areas and can change the styles of text.
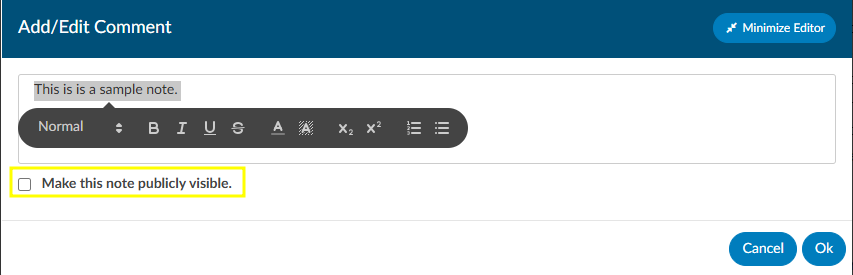
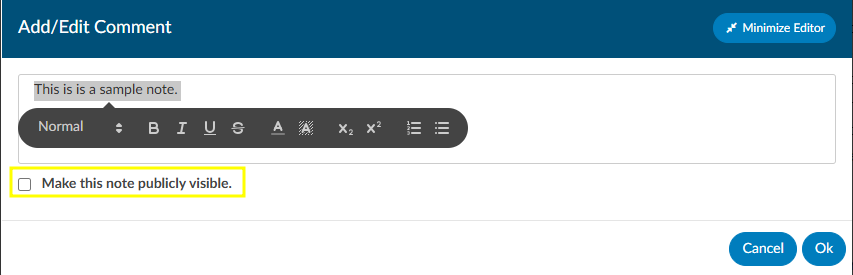
Users have the option to make notes publicly visible among all users by clicking on the checkbox. Even if an end user marks a note/bookmark as private, users with the role of administrator or manager can still see private comments. This feature allows for a manager to review a patient chart and if they do not want the existing public note to show in the account note, they can change an existing note to private without putting in a new note. Then they have to make it public, then switch it to private in order to have the account note blank.
To keep your Comment box open while continuing to work on the chart, click on the Minimize Editor button. This will move a placeholder to the Accounts Action Bar.


Bookmarks
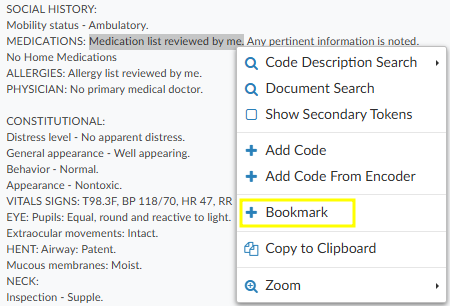
Users can add a bookmark to a document by highlighting the relevant word(s), phrase or location within the text and then right-clicking to open the Bookmark menu.
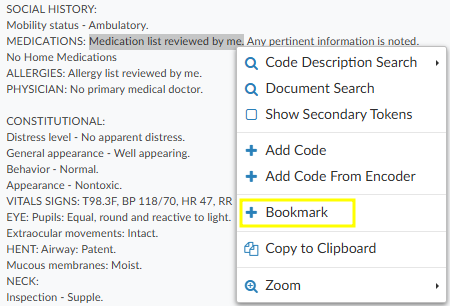
From the Bookmark menu, select Bookmark to open the Note window to add your note for this bookmark.
Add the note for your bookmark in the Note text box, then click the checkmark button to save the bookmark with your note for future reference. Bookmarks within documents will have the bookmark icon. To view bookmarks from within a document, click on the green icon to open and view the bookmark note.


To review all bookmarks within a chart, go to Notes & Bookmarks in the Navigation tree. All of the bookmarks within the chart are listed in the Notes & Bookmarks viewer.
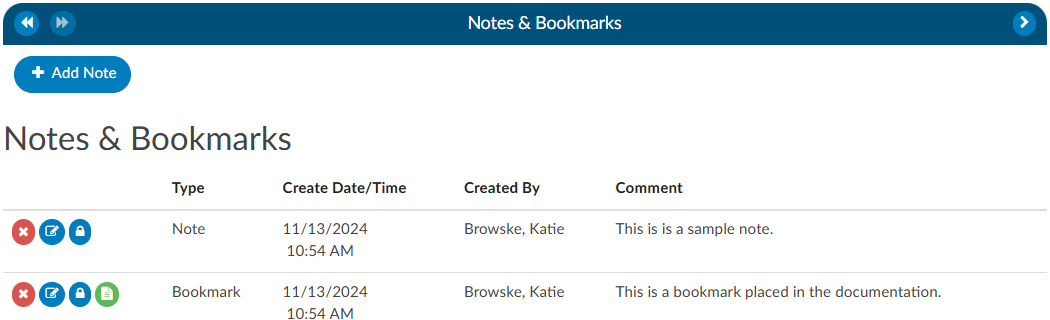
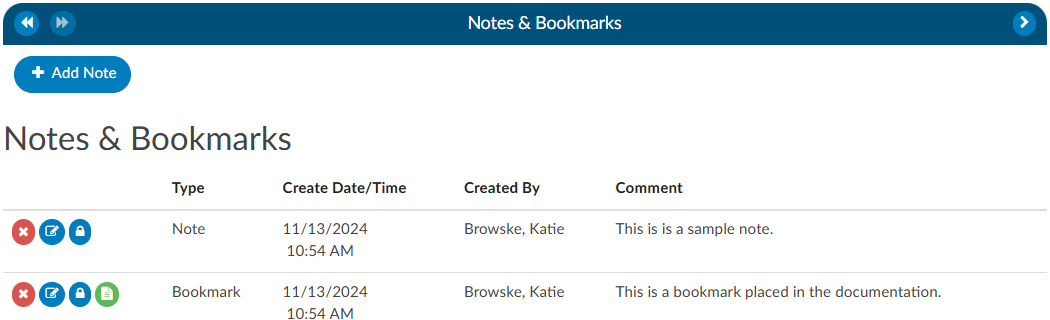
The RED X
button will delete the selected bookmark.
The BLUE PENCIL
button is used to edit a previously added bookmark.
The GREEN PAPER
button will jump to the location where the bookmark was created.
Physicians & Queries
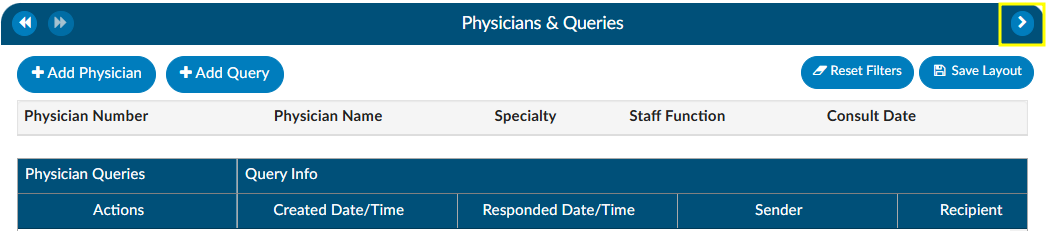
Within this viewer users can add physicians and change the physician’s staff function, if necessary. They can also intiaiate the physician query process in this viewer. Users can expand the width of the Physicians & Queries viewer by clicking on the arrow in the top right corner of the viewer.
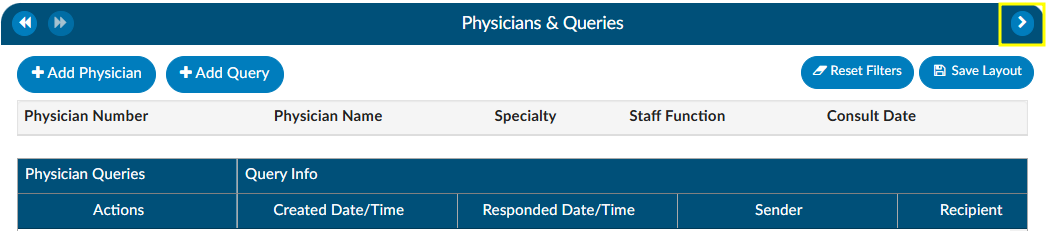
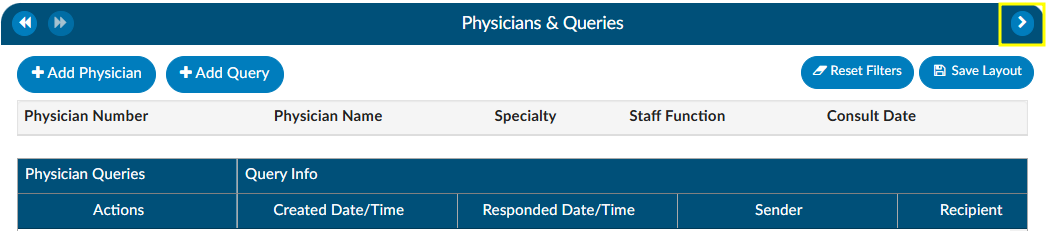
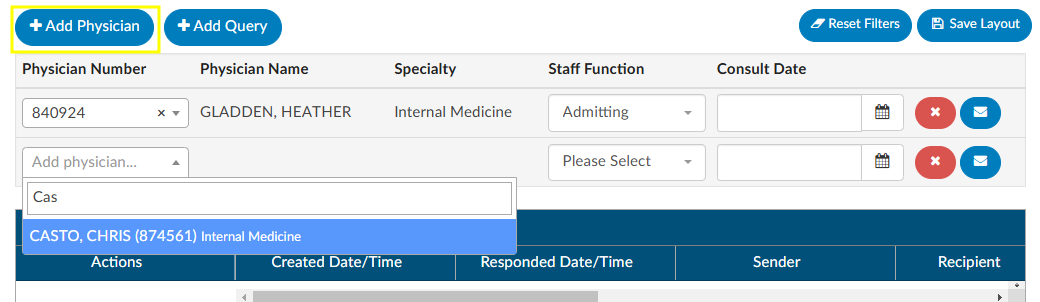
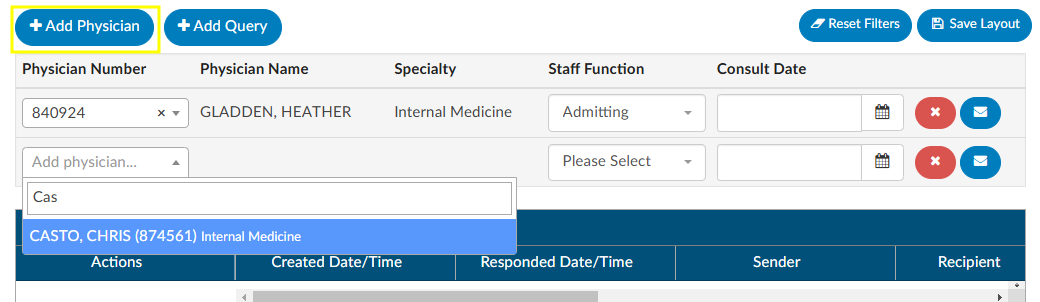
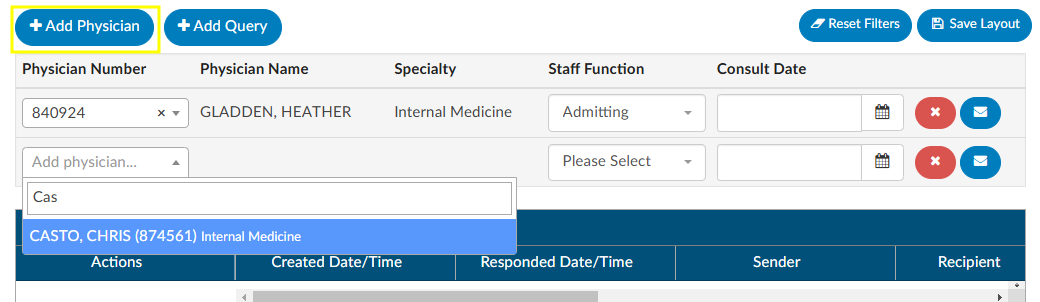
Adding/Editing Physicians
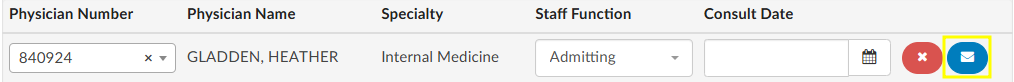
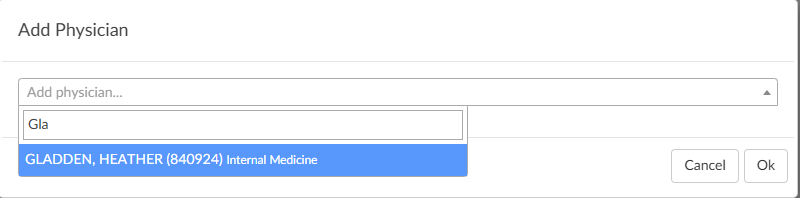
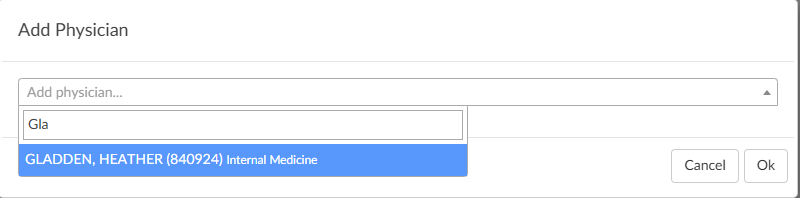
The are several fields that are pre-populated by the organization’s registration system including “Physician Number”, “Physician Name”, “Specialty” and “Staff Function”. Physicians can be added, changed, or removed if incorrect or missing. To add a physician, click on the +Add Physician button and begin typing in the physician’s last name to populate the correct physician. Choose the staff function that fits the chosen physician. If it is a consulting physician, also enter the consultation date.
To remove a physician that either you added or was sent incorrectly from the registration system click on the RED X button to remove the physician.
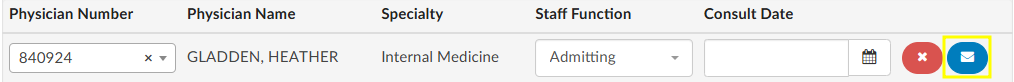
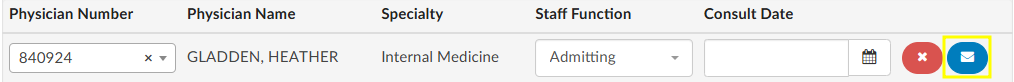
Querying a Physician
Adding a Query
There are two ways to add a query to a physician that is listed. The first is to click on the BLUE ENVELOPE
icon next to the physician.
The second way is to click on +Add Query. This would also be how to query a physician that is not already listed.
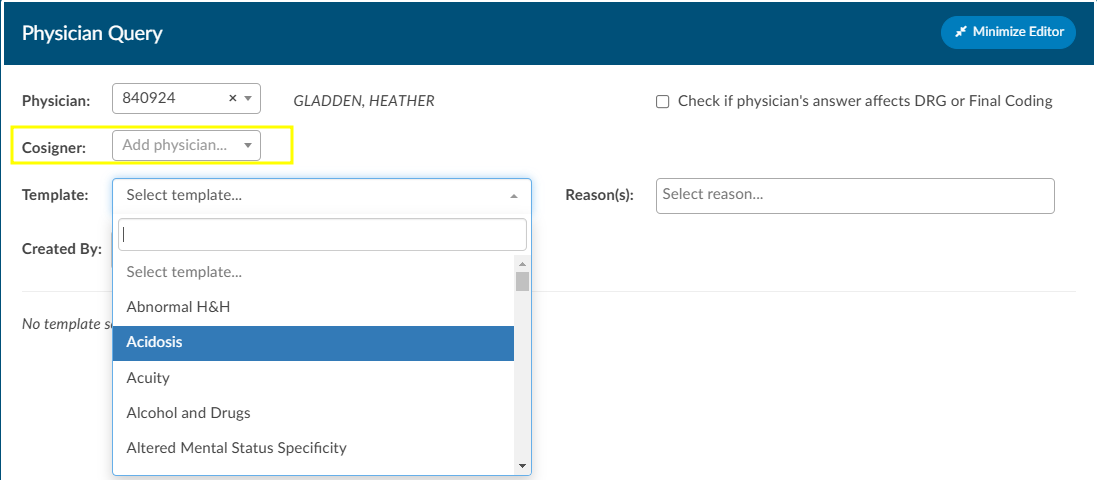
When a physician is listed, the query will auto-populate the physician name. If a physician was not already listed, simply begin typing in the last name in the “Physician” field by entering two or more characters to find the correct physician name.
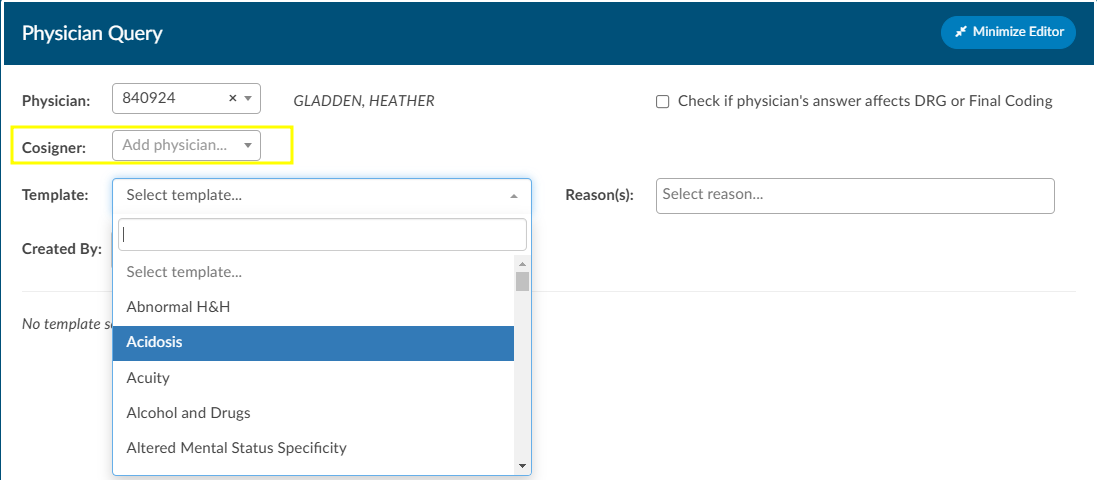
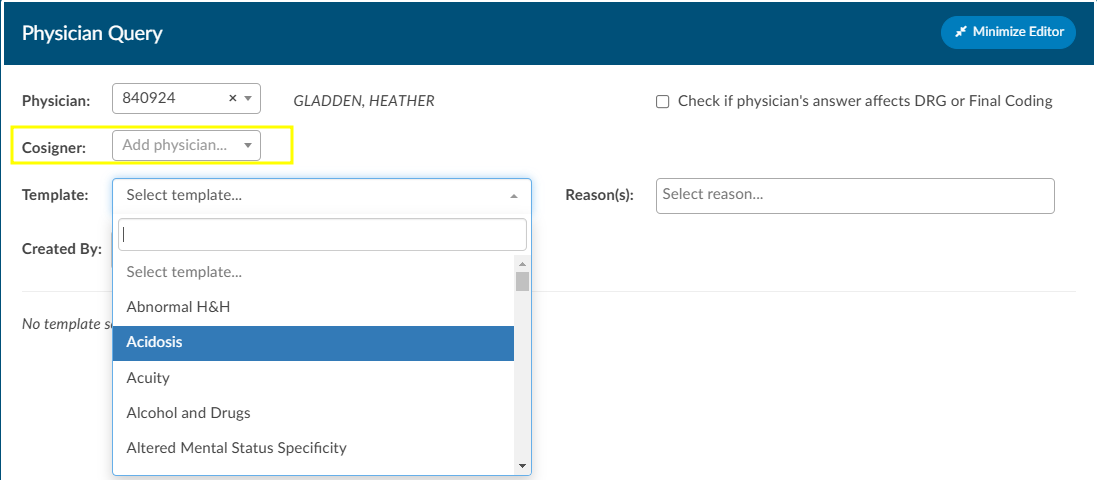
If configured, users can see a cosigner field that allows assignment of a cosigner. The cosigner field is a field that can be sent in the outbound interface for the query. The receiving system can choose to use this process if the cosigner needs to receive the query after the main recipient answers, but before it gets returned to Fusion CAC. When a physician query is created, a new “Cosigner” physician dropdown appears below the existing “Physician” dropdown. Filling in this field is optional. When the query is saved as a draft or sent outbound, the cosigner field will be saved with the query and sent as an additional recipient. In the grid inside the Physicians & Queries, the user may also choose to add “Cosigner” as a visible column.
Continue through the query build by selecting the query template.
Sending a Query
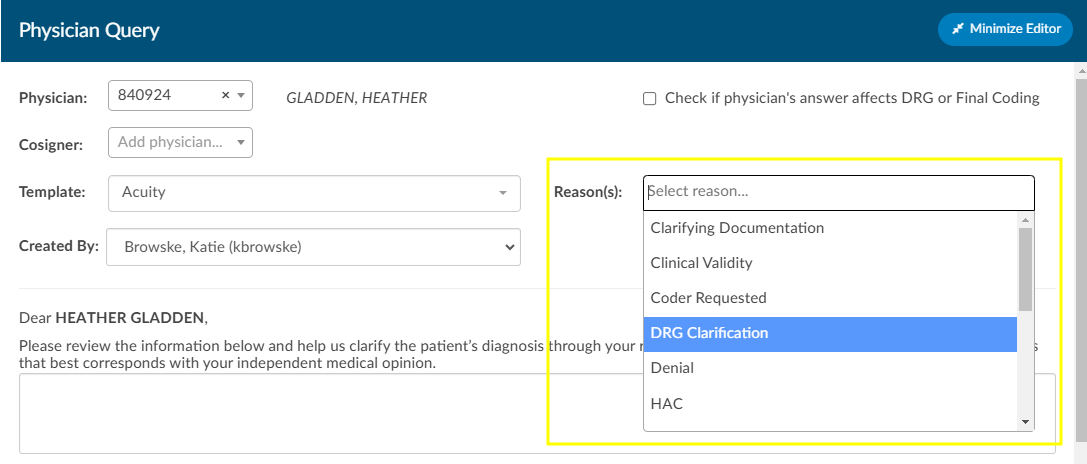
Write the query or fill out the template details as needed.
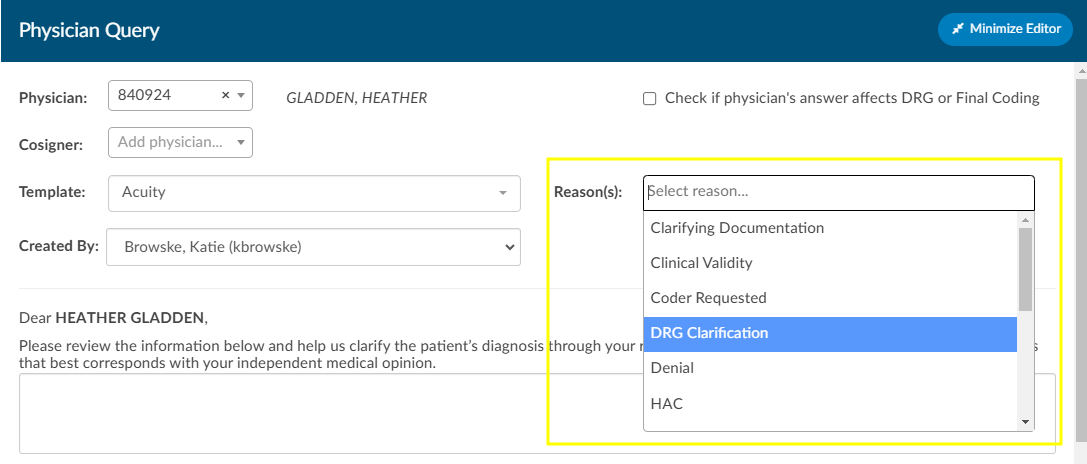
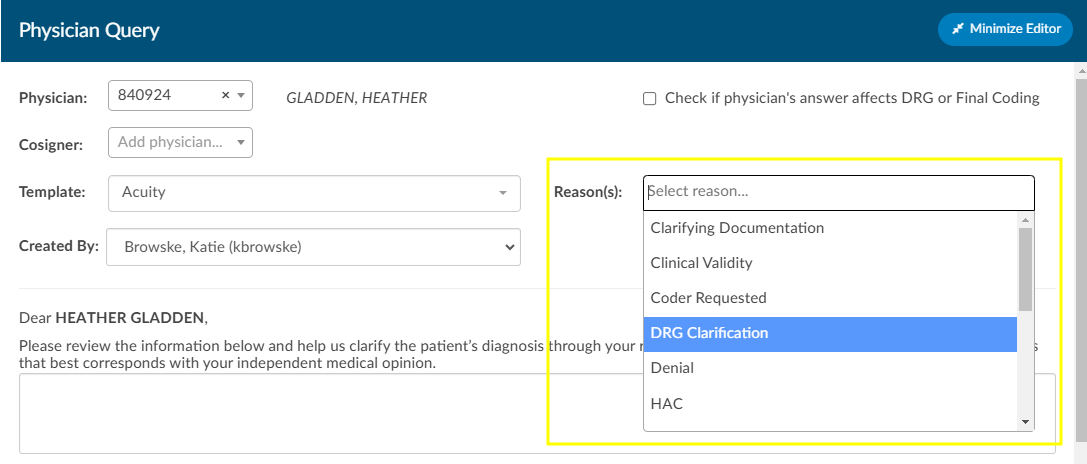
Once completed, select from the reason dropdown why you are sending the query, and above that field, check the box if the query will affect final coding.
Checkbox
The checkbox “Check if physician’s answer affects DRG or Final Coding” will not be visible to providers.
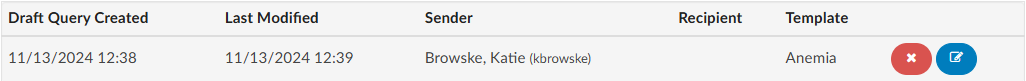
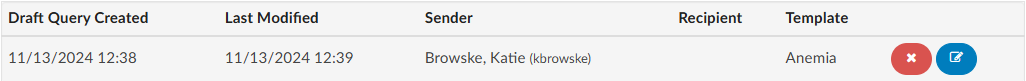
Click Send to Physician to complete the query and send it, or click Save Draft if the query is not ready to be sent. If the query is saved as a draft, a draft query section will appear that is separate from sent or closed queries. If a user has at least one draft, but no sent queries, the total drafts count on their personal dashboard will display as zero.


Alternatively, for organizations who do not have a physician query interface AND do not create a physician query until a response is received, a query can be created and not sent. When enabled, a physician query will show a Continue button in place of Send. Clicking Continue will refresh the query to open the physician response fields so that the query can then be closed.
Editing a Sent Query
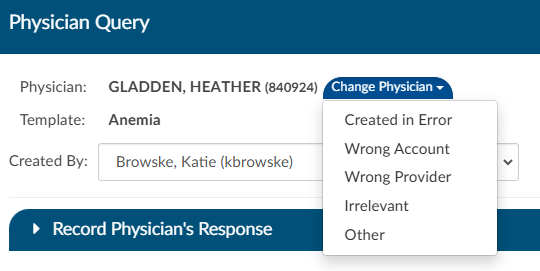
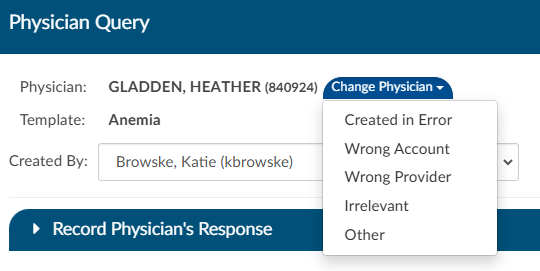
The physician the query was orginally sent to can be changed after sending the query by opening the query and clicking Change Physician. A dropdown will appear so the user can select the reason the physician needs to be changed.
Closing a Query
To close a query—whether to review a response and update the outcome or to cancel it—simply click the RED ENVELOPE
icon. If a response from the provider is available, clicking the icon will open the query to display it.
The user can then choose how to close the query using options in the screenshot below.


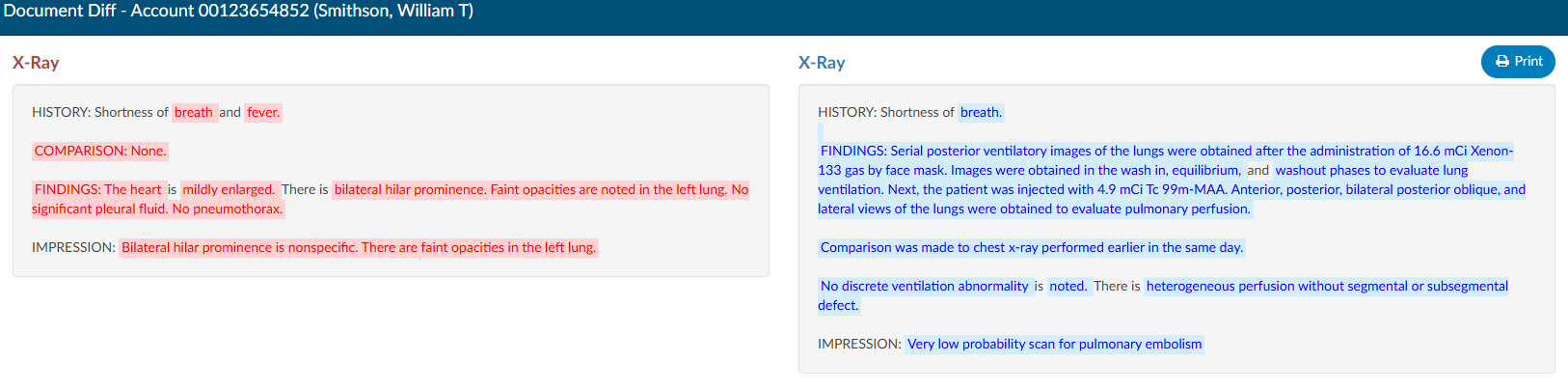
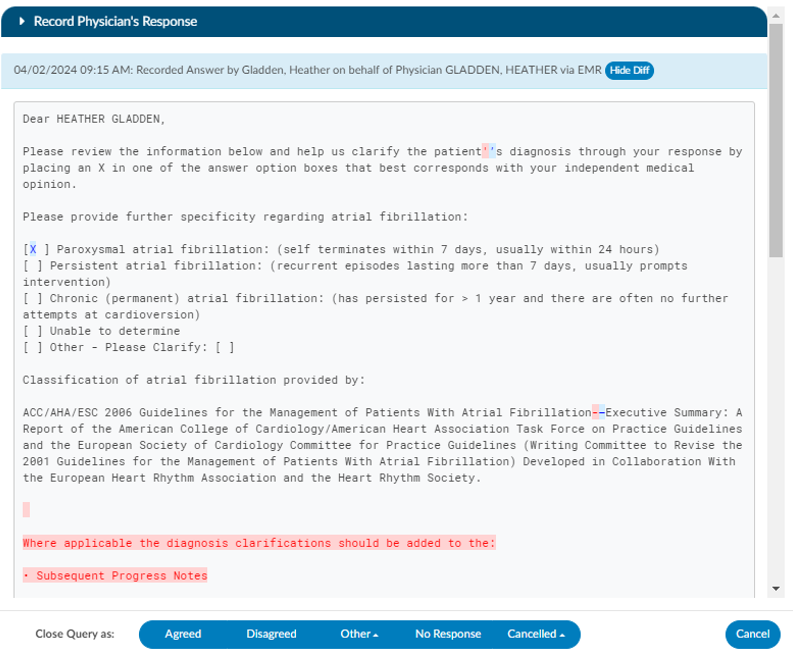
Query Response Show Diff
The physician query has a “Show Diff” toggle above physician query responses in the Physician Query dialog. Clicking it will show additional text in blue highlighting and deleted text in red highlighting. When the diff is shown, the button changes to “Hide Diff,” which when clicked will show the unaltered response.
Diff Logic
If your organization has an interface that imports the physicians response, the diff logic may report false positives and false negatives, like changes from double quotes to single quotes or the addition/deletion of blank lines.
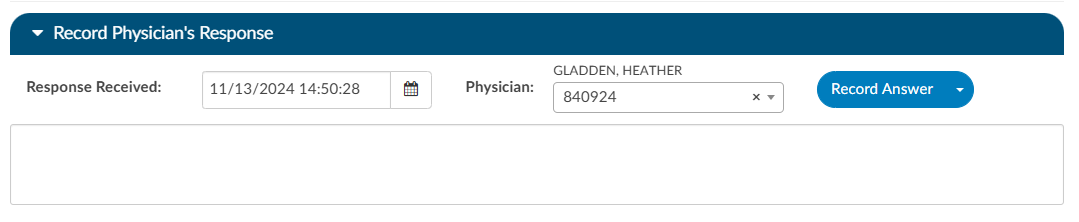
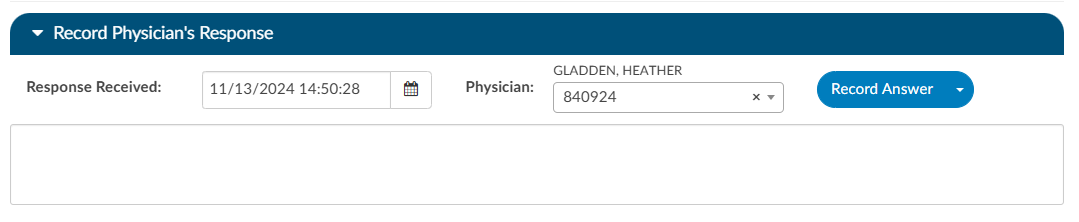
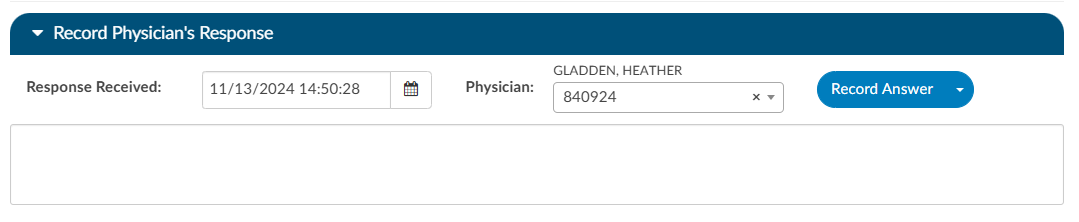
Once a query is opened and responded (or the user is recording the response on behalf of the physician), the responding physician and the date/time of the response can be editied. If the organization is manually closing queries, this information ensures that the management reports reflect accurate turnaround times.
If an organization has choosen to collect shift reasons, a dialog box will appear upon selecting an outcome for the query.
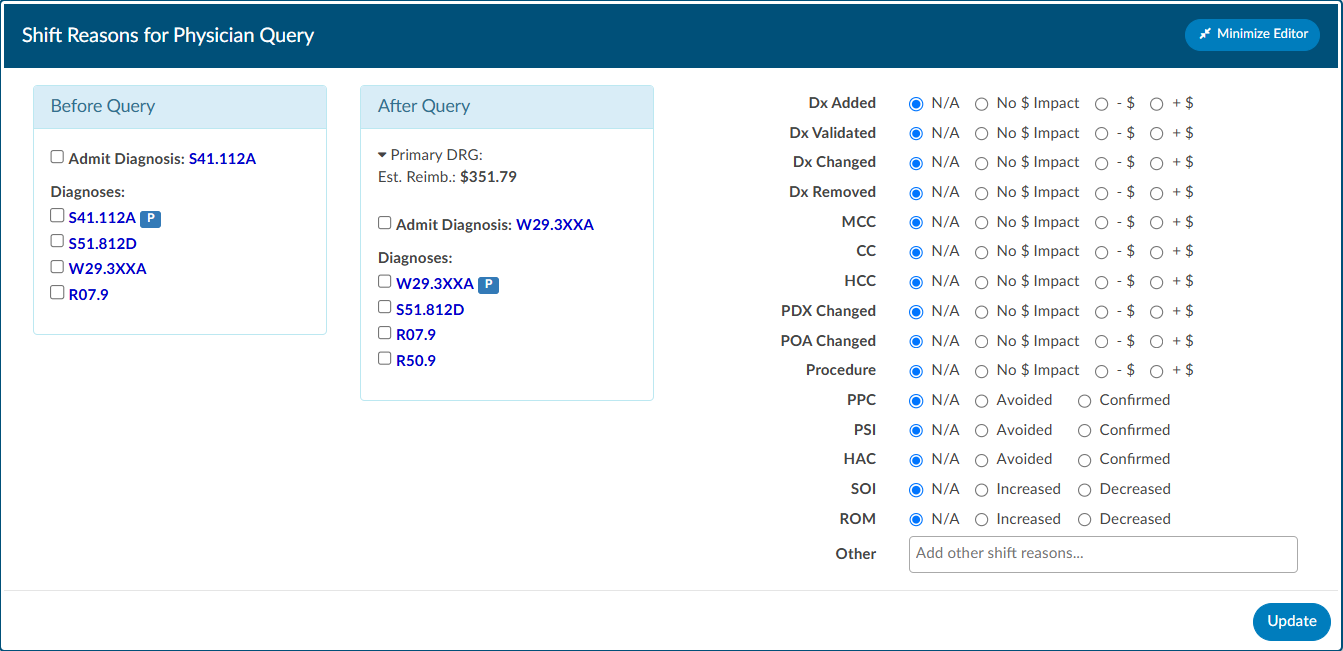
Documenting Query Shift Reasons
Shift reasons can be categorized as either automatic or manual. If manual shift reasons are enabled, users will encounter a dialog box after closing a query.
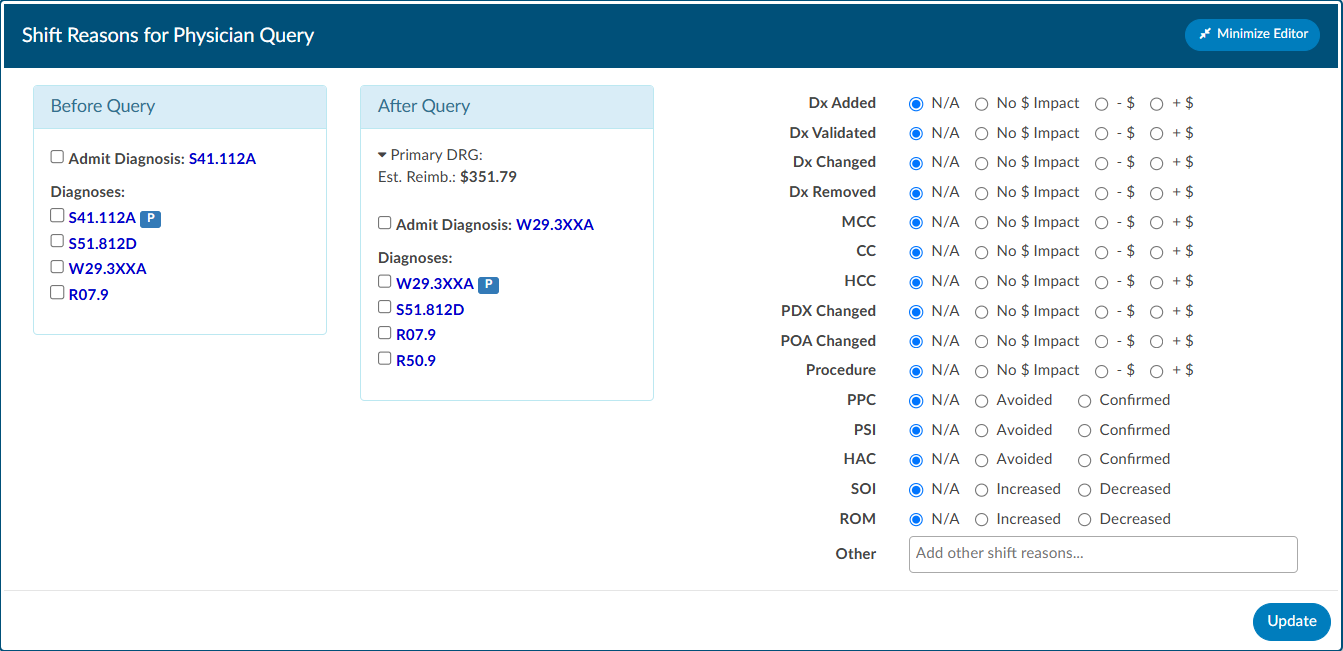
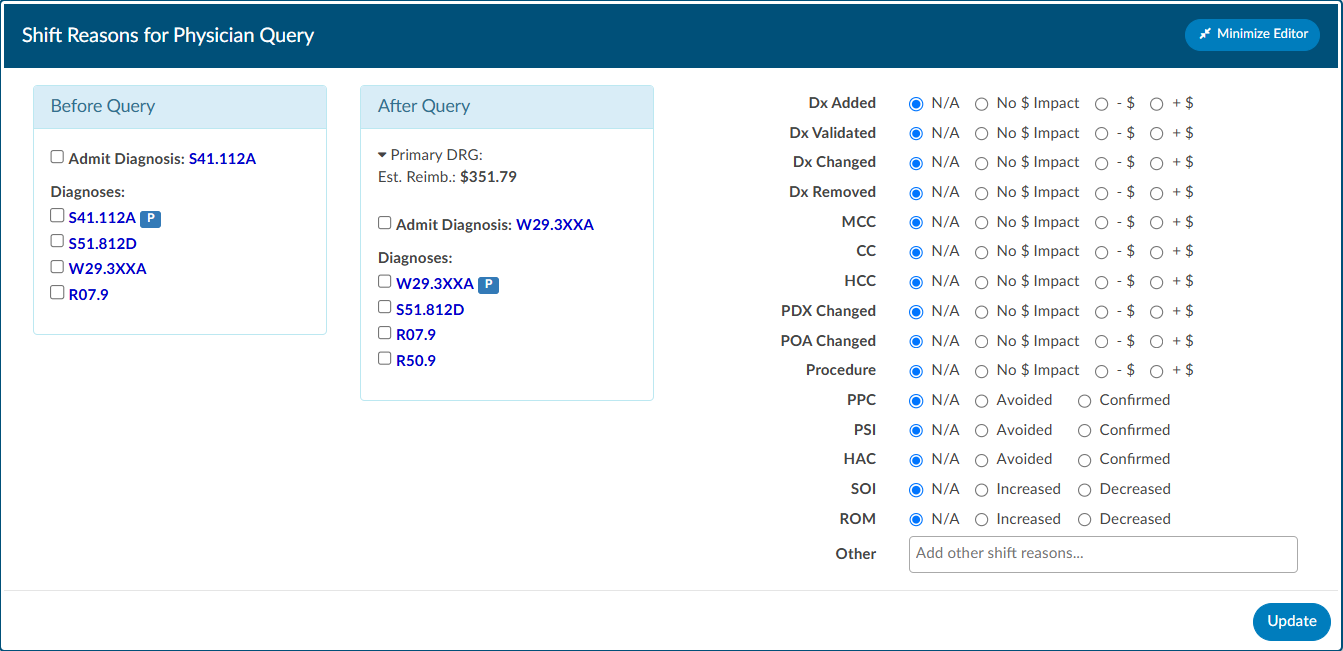
This dialog box will display the pre and post-query DRG (if applicable) along with options for shift reasons. These shift reasons can be chosen by the end user to explain the rationale behind the change in the DRG. It is important to note that changes in the DRG might occur for reasons unrelated to the query outcome. Please be aware that the shift reasons dialog is customizable, so each organization may offer different options than what is shown in the screenshot.
Automatic vs Manual Shift Reasons
The dialog box will only display if shift reasons are set to manual. Organizations looking to enable or disable the dialog box, should contact CAC Support (cacsupport@dolbey.com)
Query Impact
Query Impact = Pre-Query Working DRG Weight – Post-Query Working DRG Weight
Query impact is calculated using the working DRG calculated within the same session in which the physician query was created. Once the
physician replies to the query, the CDI will close the query. During the session the query was closed, the system will then capture the working DRG that was calculated. A session is closed by saving the chart.
If a physician query shifts the assigned DRG, diagnosis, procedures, CC/MCC/HAC/ROM/SOI or Quality
metrics, the shift reason is automatically calculated by the system. The shift reason is captured by looking at the difference between the last working DRG and the Current Working DRG as well as the Code Sets difference in the most current working DRG. Code sets will be automatically captured for reporting.
Upon initiation of the query, the user will see a Compute button below the template name. Click to compute the Pre-Query DRG if not already showing. Clicking this button will use currently assigned codes on the chart to compute a DRG. Once the pre-query DRG is completed users will follow the standard process to send the query.
When the query has been responded to, open the query to complete by clicking the RED ENVELOPE icon. Users will be able to compute a post-query DRG in order to capture impact. The previous DRG will auto-populate (unless the user added, deleted, or changed any codes, re-sequenced or changed the discharge disposition). If the pre-query DRG does not populate, it will need to be calculated again by clicking the Compute Pre-DRG below the template name. Users will now also see a Compute Post-DRG below the template name.
Users can minimize the query as needed to add, delete, or otherwise change any codes before clicking compute.
Placeholder Queries
Some organizaitions create a physcian query within Fusion CAC and then copy and paste it into a different system rather then send them through an interface. Dolbey refers to this as a place holder query for reporting and transparencey. A feature can be enabled so that text entered into fields on the place holder query will no longer display in bold. To activate this option, please contact CAC Support (cacsupport@dolbey.com).
Quick Complete
The Quick Complete query feature is designed for sites that create placeholder queries ONLY. This feature allows a user to log a query without sending it externally. The user can assign a provider, template, reason, and both pre and post-DRG information along with closing the query with shift reasons all in one session. This quick complete feature aims to streamline these actions into a single, integrated process. This feature is optional and needs to be turned on. Contact CAC Support (cacsupport@dolbey.com) to enable this feature.
Once enabled, create a new physician query, and notice a new Quick Complete button in the footer. Clicking it will automatically save the query and reopen it with “Record Physician Response” expanded to record a physician’s response. The Quick Complete button only appears on new queries, including queries opened from drafts. It will not appear if a query is edited or if a query’s physician is changed.
Query Status
The status of the query will display in the actions column on the query grid. The following are status options:
| Status | Description |
|---|
| Open | This query has been sent, but not yet responded to by the provider. |
| Answered | This query has been sent and has received a response, but has yet to be closed by the end user. |
| Canceled | This query has been canceled by the end user. The status column will display the reason for the cancellation. |
| Closed | This query has been closed by the end user. The status column will display the outcome of the query. |
Canceling Queries
Not all organizations support canceling physician queries. Redirected queries may still need to be canceled within the EHR. Consult your supervisor to learn if additional steps need to be taken to cancel a query.
Per User Settings
This grid will display key details about the query, including the creator, recipient, creation date, reply status, and response timestamp. Columns can be reordered based on user preference. When moving around the columns in the Physician Queries grid and then clicking the Save Layout button, the columns and order will be saved for the Queries grid for all future accounts for that user. Any other user will see the default layout. Next to the Save Layout button is a Reset Filters button, this will take any custom layout and change it back to the default fields.
If the organization chooses to use signatures when sending queries, automatic signatures can be addended to the query. Signatures can be editied within each user’s profile.
Note
Please refer to your supervisor for details as each organization has custom query templates and additional details surrounding queries.
Previous HCC
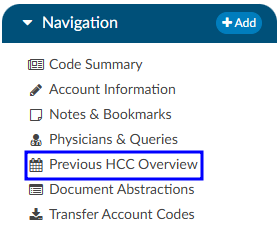
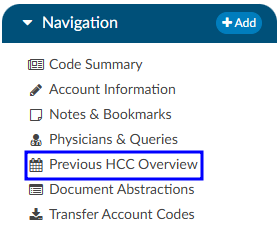
The Previous HCC Overview will display the HCC history to show for both the current and prior year. When HCCs are enabled, these will display grouped by HCC category and by code — showing the account number and MRN for the visits each were associated to.
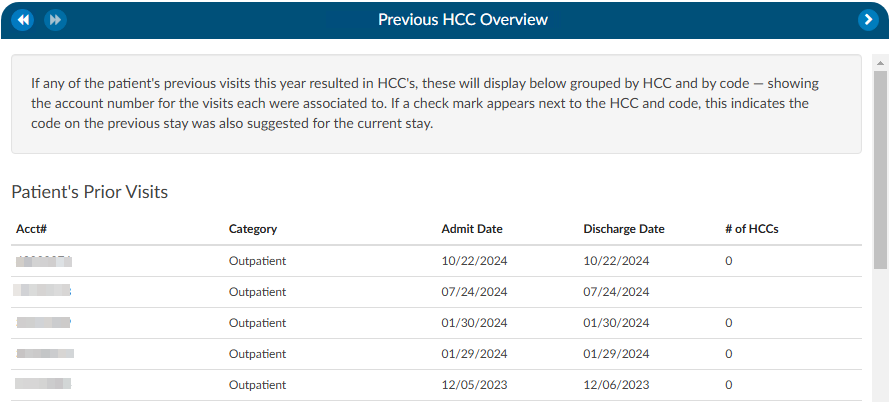
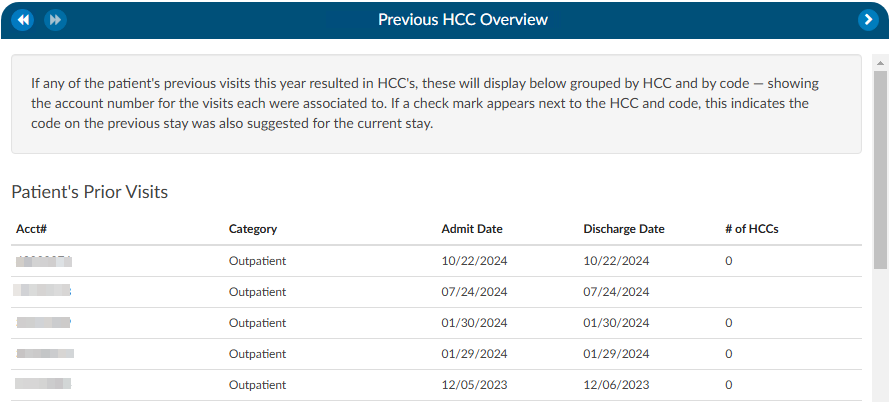
If a check mark appears next to the HCC category and code, this indicates the code on the previous stay was also suggested for the current stay. If the patient chart currently being coded has codes that result in HCCs once they are added to the assigned code tree the code will display with an ‘H’ next to the code. By hovering over the ‘H’ icon, the HCC category will display.
It is recommended to turn HCCs on for all patient types to capture a more complete picture of HCCs. HCCs will be collected once HCCs have been enabled in the mapping table. To enable HCCs, check the box in the Category mapping table.
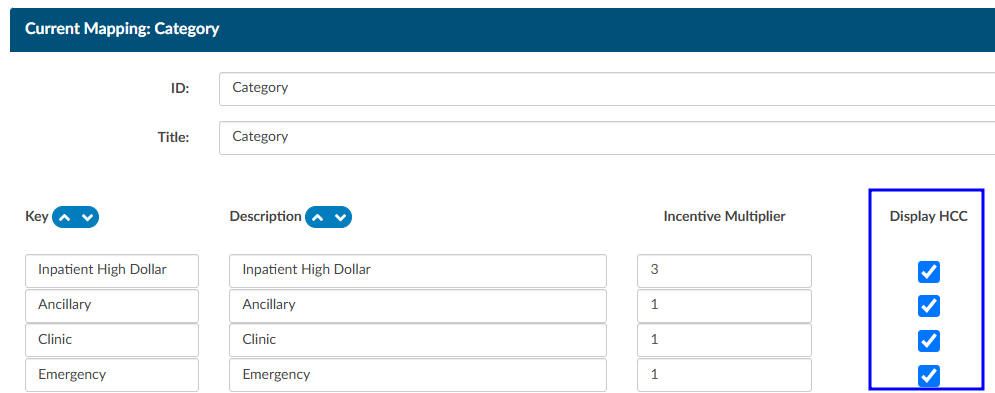
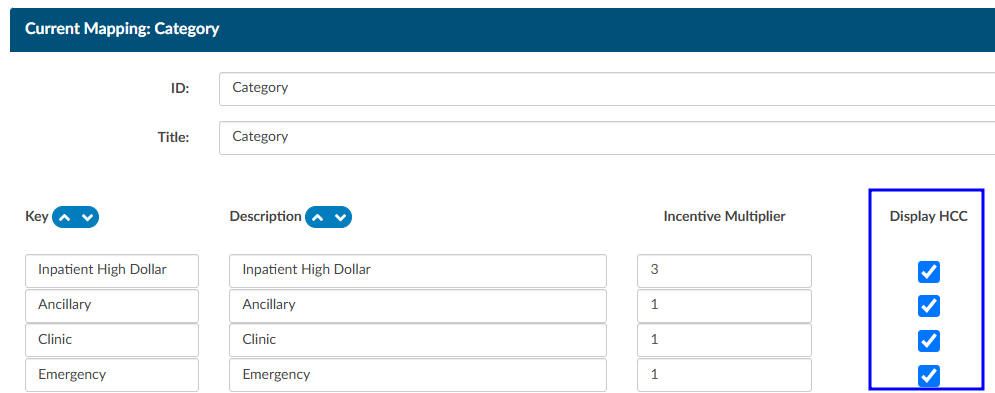
As a reminder, this will not capture data prior to turning this feature on in the mapping table.
Readmission/Previous Visit
If the patient has been readmitted within 30 days of an admission date, the patient demographic data will display below from the previous stay. This is not just for inpatient readmissions, but also includes if the patient was ever seen for any patient type within the last 30 days. The 30 days look back can also be expanded to 45 or 90 days. If the previous stay was also coded, you will see the Code Summary display below. If a check mark appears next to the code, this indicates the code on the previous stay was also suggested for the current stay.
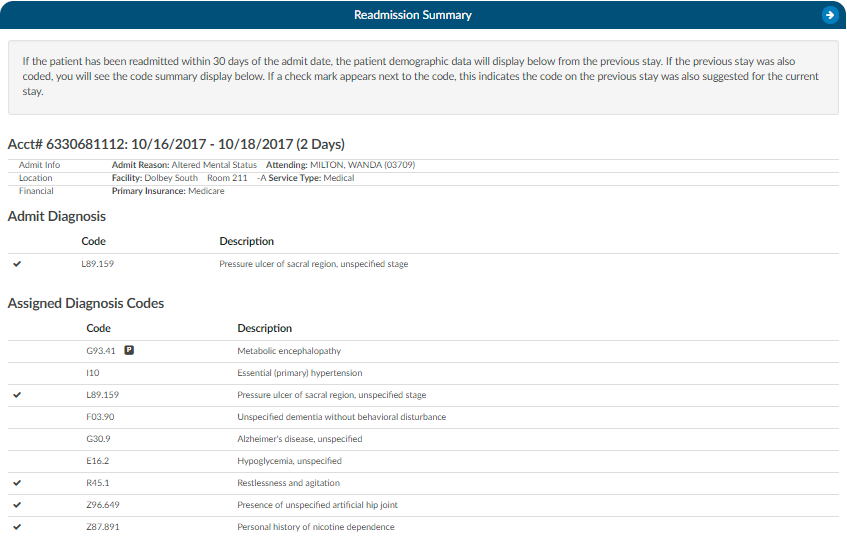
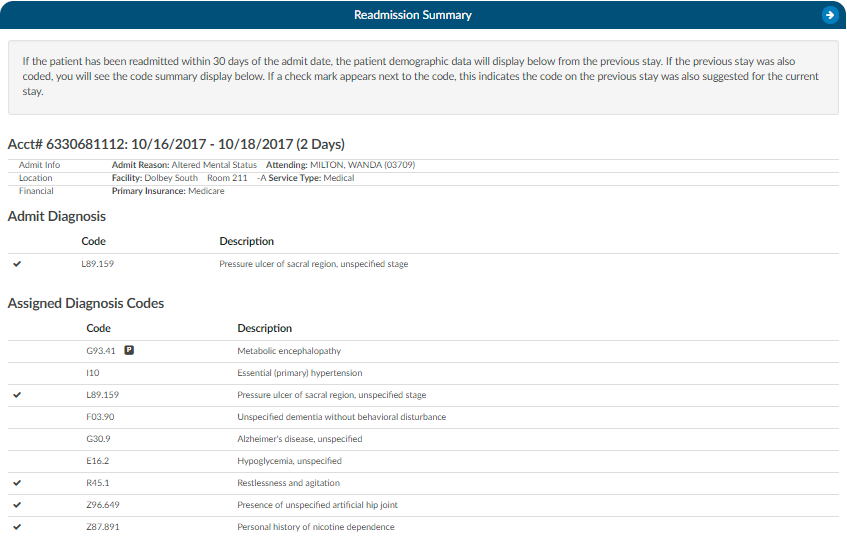
If an account has multiple re-admissions, they will all show if they are in the default time of 30 days. A setting can be changed to allow the number of days to be customized. If the setting is updated to an amount other than 30, that new amount will show in the Re-admission Viewer AND in the red tag in the banner. Please contact Support (cacsupport@dolbey.com) to have the setting configured, if desired.
Time Tracking Viewer
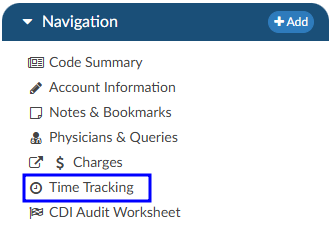
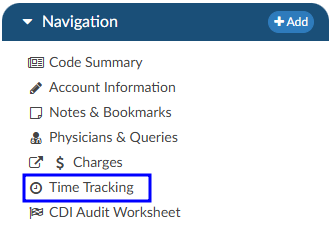
The Time Tracking Viewer allows for time-tracking on four types of documents:
- Denial worksheets
- Audit worksheets
- Documentation Reviews
- User added worksheets
The above worksheets will be read only until the Start button in the top right corner of the worksheet is clicked.


Tracking will be stopped when:
- The user clicks the Stop button


- The user opens another document and starts its time tracking
- The user exits the account
Users will be able to adjust their time in the Time Tracking viewer if necessary. Managers and admins can view time tracking data for all users; however, each user is only permitted to edit their own time entries. If a time entry needs to be corrected, the manager or supervisor must ask the individual user to make the necessary changes.
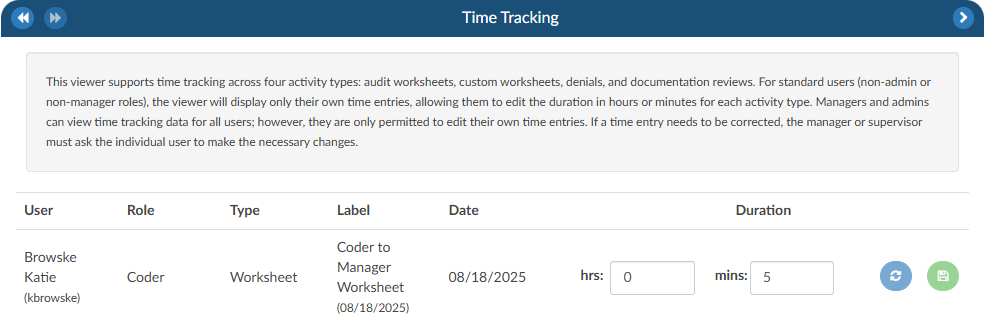
Transfer Account Codes
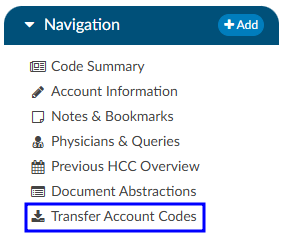
Transfer codes can be used to help combine account codes into one encounter. Most sites leverage the ADT to combine the actual account; however, there are times it is necessary to copy codes from one encounter to another.
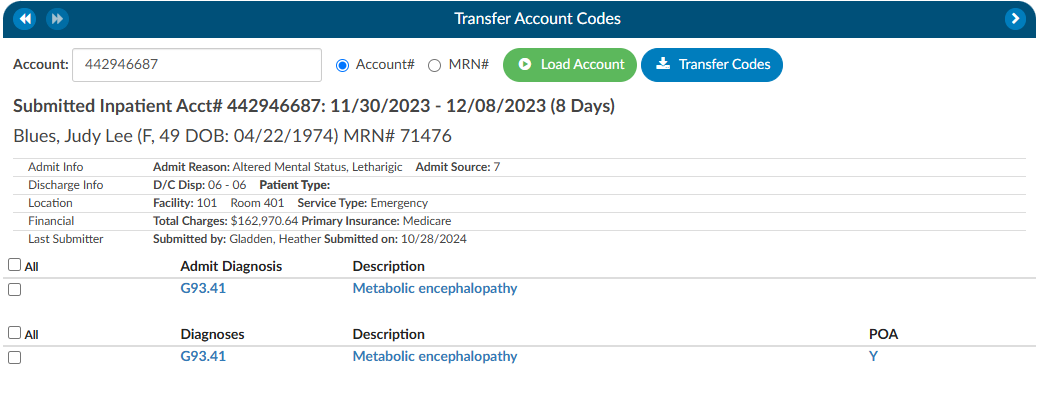
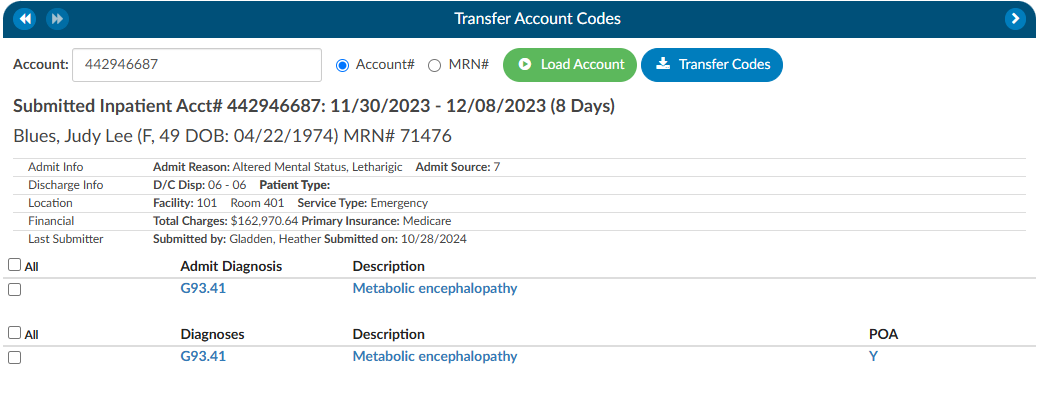
If a patient has two different accounts and the coder has already done work on each of the accounts, the Transfer Codes feature can be an easy way to post codes when you’re within one account and want to search in another account, and have the ability to open that other account and see the codes.
To transfer codes either select the Account# radio button and type in the account number, or select the MRN radio button where the MRN of the opened account will populate. Once either of those numbers are entered, click the Load Account button. When the account or MRN is loaded, use the check boxes to the left of the codes to choose which codes will transfer. Once the needed codes are checked, click on the Transfer Codes button and the codes you selected will be added to the “Assigned” codes tree that is on the current account.
Working CDI History
The working CDI History can be used to look at historical working DRG calculations. The Coders cannot edit this information, but they can review the data.
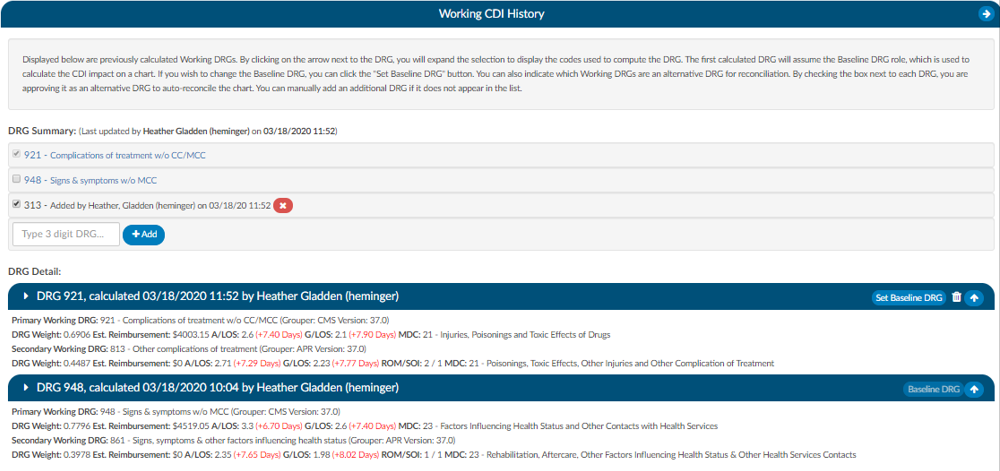
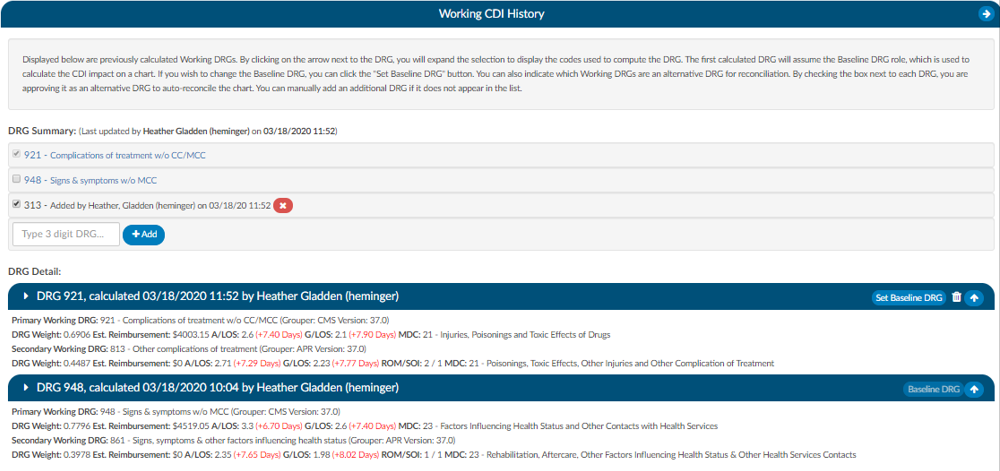
The first calculated DRG will assume the Baseline DRG role, which is used to calculate the CDI impact on a chart. Users wishing to change the Baseline DRG, can click the Set Baseline DRG button.
Users can also indicate which Working DRGs are an alternative DRG for reconciliation. By checking the box next to each DRG, users are approving it as an alternative DRG to auto-reconcile the chart. Users can manually add an additional DRG if it does not appear in the list.
Clicking on the arrow prior to the DRG information will expand the selection to display the codes that went into the DRG and the sequence. Any codes with a plus sign indicates the code has not been added to the account. The plus sign does not indicate that the codes need to be added. It simply allows the user to quickly add the code if they have determined it is vaild using their coding judgment and supporting documentation. If applicable, the code’s HCC designation will show the HCC number and its version.